Working with Survivors of Sexual Violence Presents Unique Challenges
PAs Should be Aware of Complicating Factor for Patient Health
November 25, 2020
By AAPA Research Department and Katherine M. Thompson, MCHS, PA-C, FE
Sexual violence affects every demographic and every community, making it a serious public health concern. Proper identification of sexual violence and treatment is the first line in positive patient outcomes. Often underreported, failure to identify and treat patients can lead to chronic physical and psychological problems.1 Sexual violence is defined as any unwanted sexual contact, including words and actions of a sexual nature against a person without their consent.2 Sexual violence is not a crime of sex but one of power and control.
Nondisclosure of sexual violence is associated with poor levels of health. 3 Affecting nearly 600,000 individuals every year in the United States, sexual violence is defined by the CDC as sexual activity when consent is not obtained or freely given.4 With most perpetrators known to the victim, meaning it could be a friend, current, or former intimate partner, coworker, neighbor, or family member, this act of violence is one of the most common forms of violence any community will face. According to RAINN (Rape, Abuse, & Incest National Network), 80% of all rapes are committed by someone the victim knows and 93% of all sexual assaults to children were known by the youth.5
How common is sexual assault?
 Over 400,000 people aged 12 and older reported being sexually assaulted or raped in the U.S. every year; 60,000 children were victims of “substantiated or indicated” sexual abuse, 80,000 inmates, and close to 19,000 military personnel reported unwanted sexual contact.5
Over 400,000 people aged 12 and older reported being sexually assaulted or raped in the U.S. every year; 60,000 children were victims of “substantiated or indicated” sexual abuse, 80,000 inmates, and close to 19,000 military personnel reported unwanted sexual contact.5
In terms of lifetime prevalence of sexual assault:
- 1 in 3 women and 1 in 4 men have experienced some form of unwanted sexual contact; 1
- 1 in 8 women and 1 in 15 men reported sexual coercion; 1
- 1 in 5 women and 1 in 18 men have experienced sexual violence involving attempted or completed rape; 1
- 1 in 14 men reported that they were made to penetrate someone else; 1
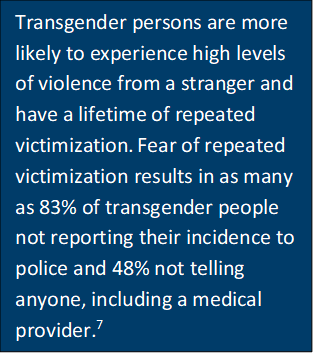
- 1 in 8 lesbian women and half of bisexual women reported completed rape;6 and
- 4 in 10 gay men and nearly half of bisexual men have experienced sexual violence. 6
 Why is it hard to measure?
Why is it hard to measure?
Sexual violence is difficult to measure. Currently, there is no single source of data that compiles all statistics. As the crime is often underreported, estimates of the total numbers of those affected fluctuates between agency sites. Some experts believe that just 25% of all incidents are reported to the police. The introduction of behaviorally-specific questions, health context, and common-language usage have reduced some barriers to reporting.1 The sensitivity of the subject still may be an inhibiting factor for victims and it is highly likely that national statistics underestimate the number of sexual violence victims per year.
How does sexual violence impact the health of patients?
The reporting of sexual violence can often be a traumatizing experience for victims and can compound the effects of sexual violence. Negative impacts on psychological, emotional, and physical well-being of the individual can occur and are difficult to manage without the proper care and support networks. It is critical for healthcare providers to be aware of sexual violence as a complicating factor for overall health and wellness.8
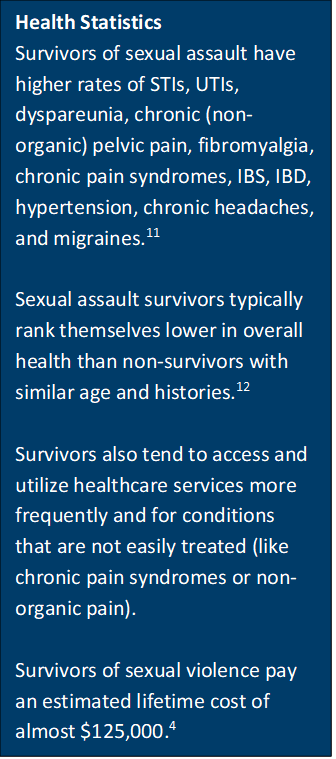
Depression, anxiety, and post-traumatic stress disorder (PTSD) are among the most common forms of psychological responses victims face.9 Reigning theory in pain management and pain syndromes suggest that an unknown majority of patients who have chronic pain syndromes and similar conditions likely have a history of sexual assault or sexual violence.10
Additional concerns with reported and unreported sexual violence are sexually transmitted infections, pregnancy, eating disorders, sleep disorders, and coping mechanisms like disassociation and substance abuse.13 Community stigmas and fear of health professionals may be a contributing factor for the higher rates of recovery problems faced by women who are bisexual and women who are minorities.14
Recognizing the root cause of many conditions that PAs commonly treat will help victims become survivors and will help to establish better records of sexual violence numbers. Adopting Trauma-Informed Care (TIC) practices, often called the “Four R’s” acknowledges the trauma and the role of trauma in a patient’s life. This acknowledgement of trauma helps practitioners aide their patients’ recovery and discover more victims and survivors of sexual violence.15
[Support AAPA’s original research on the PA profession – join or renew today]
What can PAs do?
There is a strong forensic network for acute assault in the U.S. – albeit weaker in non-urban areas – but the real failure is in late disclosures and detecting sequelae long-term. In most health systems providers do not ask about sexual violence history, and those who do are generally in specialties such as obstetrics and gynecology, primary care, emergency medicine, and urgent care.
Data from the May-June 2019 AAPA PA Practice Survey showed that nearly half of all PA respondents had not received any training on the treatment or management of sexual violence survivors. Of those that had received training, 82% had lecture-only training with fewer than one-fourth of those having any practical knowledge. In the needs assessment, all six questions found similar results in current versus desired skills. One-fourth to one-half of all respondents reported no skills or abilities to treat various conditions or victims of sexual violence crimes. Surprisingly, the only skill that half of the respondents wanted was in treatment of post-traumatic stress disorder (PTSD). For even more data, see the full report.
 PAs can improve their ability to treat all survivors of sexual violence through continuing education and in adjusting practice habits to ask patients at every visit about their sexual health and safety. Approximately 37% of PAs were already self-educating and expanding their knowledge and providing resources in their offices or places of work to assist patients who may otherwise withhold information from their care provider. See the exact breakdown of PAs current versus desired skills here.
PAs can improve their ability to treat all survivors of sexual violence through continuing education and in adjusting practice habits to ask patients at every visit about their sexual health and safety. Approximately 37% of PAs were already self-educating and expanding their knowledge and providing resources in their offices or places of work to assist patients who may otherwise withhold information from their care provider. See the exact breakdown of PAs current versus desired skills here.
References
- Violence Prevention: What is sexual violence? Center for Disease Control.https://www.cdc.gov/violenceprevention/sexualviolence/fastfact.html Updated January 17, 2020. Accessed April 15, 2020.
- About Sexual Assault. National Sexual Violence Center: https://www.nsvrc.org/about-sexual-assault. Accessed April 15, 2020.
- Levy AG, Scherer AM, Zikmund-Fisher BJ, Larkin K, Barnes GD, Fagerlin A. Assessment of Patient Nondisclosures to Clinicians of Experiencing Imminent Threats. JAMA Netw Open. 2019 Aug 2;2(8):e199277. doi: 10.1001/jamanetworkopen.2019.9277.
- Violence Prevention: Fast Facts. https://www.cdc.gov/violenceprevention/sexualviolence/fastfact.html. Updated January 17, 2020. Accessed March 30, 2020.
- Scope of the Problem: Statistics. RAINN. https://www.rainn.org/statistics/scope-problem Accessed April 15, 2020.
- Centers for Disease Control and Prevention. NISVS: An Overview of 2010 Findings on Victimization by Sexual Orientation. https://www.cdc.gov/violenceprevention/pdf/cdc_nisvs_victimization_final-a.pdf. Accessed April 27, 2020.
- Stotzer RL. Violence against transgender people: A review of the United States data. Aggression and Violente Behavior.2009;14(3):170-179. https://doi.org/10.1016/j.avb.2009.01.006
- Thurston RC, Chang Y, Matthews KA, vonKӓnel R, Koenen K. Association of Sexual Harassment and Sexual Assault With Midlife Women’s Mental and Physical Health. JAMA Intern Med. 2019 Jan 1;179(1):48-53. doi: 10.1001/jamainternmed.2018.4886.
- Silver KE, Anderson RE, Brouwer AM. Emotional Responses to a Sexual Assault Threat: A Qualitative Analysis Among Women With Histories of Sexual Victimization. J Interpers Violence. 2020 Feb 26:886260520908019. doi: 10.1177/0886260520908019
- Spiegel DR, Shaukat AM, Mccroskey AL, et al. Conceptualizing a subtype of patients with chronic pain: The necessity of obtaining a history of sexual abuse. Int J Psychiatry Med. 2016;51(1):84-103. doi: 10.1177/0091217415621268.
- Golding JM. Sexual-Assault History and Long-Term Physical Health Problems: Evidence From Clinical and Population Epidemiology. Curr Directions in Psych Sci. 1999;8(6):191-194. https://doi.org/10.1111/1467-8721.00045.
- Chivers-Wilson KA. Sexual assault and posttraumatic stress disorder: a review of the biological, psychological and sociological factors and treatments. Mcgill J Med. 2006;9(2):111–118.
- Effects of Sexual Violence. RAINN. https://www.rainn.org/effects-sexual-violence. Accessed April 15, 2020.
- Sigurvinsdottir R, Ullman SE. Trauma as Predictors of Sexual Assault Recovery. J Fam Violence. 2016 Oct;31(7):913-921. Epub 2015 Dec 20. https://doi.org/10/1007/s10896-015-9793-8.
- Trauma-Informed Care. Agency for Healthcare Research and Quality. https://www.ahrq.gov/ncepcr/tools/healthier-pregnancy/fact-sheets/trauma.html. Published April 2016. Accessed April 28, 2020.
About the data
Data on training on training to treat and manage patients who are sexual assault survivors are derived from a study conducted in 2019 in collaboration with Katherine M. Thompson, MCHS, PA-C, FE.
Authors are Noël Smith, AAPA senior director of PA and Industry Research and Analysis, Kristina Medlock, AAPA Research Intern, and Katherine (Katie) M. Thompson, MCHS, PA-C. Contact Noël at [email protected] and Katie at [email protected].
Editor’s note: This article originally appeared in April 2020.
Read More
AAPA Report on PA Training on Sexual Violence
Providing Strength in the Wake of Trauma
How to Talk With Patients About Intimate Partner Violence
Human Trafficking: Become Informed and Be Attentive
More Resources
IPV Educators
US Code of Federal Regulations which defines military law, definition of rape and sexual assault
RAINN (Rape, Abuse, & Incest National Network)
American College of Obstetricians and Gynecologists (ACOG) Clinical Guidance on Sexual Assault
Agency for Healthcare Research and Quality Fact Sheet on Trauma Informed Care
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.