Crisis Plan for APPs Reduces COVID-19 Exposure and Risk
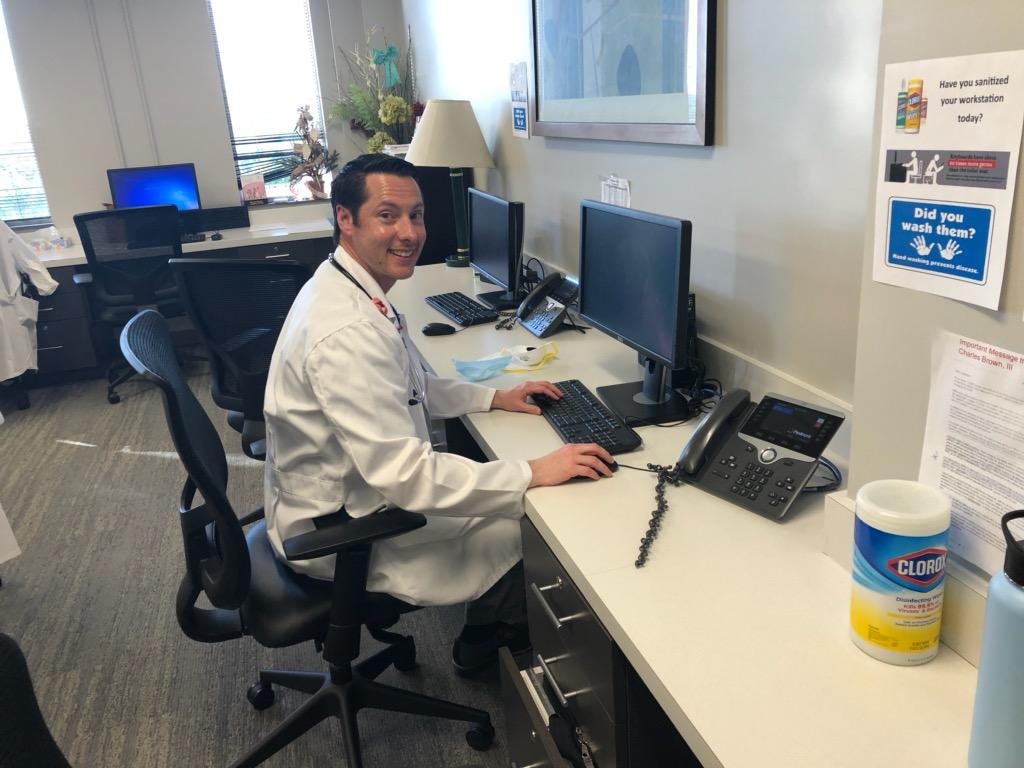
Kyle Fortman, PA-C, Develops Tips for Providing Care at Piedmont Heart Institute
By Kyle D. Fortman, MPAS, PA-C
April 15, 2020

As the Lead APP for Acute Care Services at The Piedmont Heart Institute, Piedmont Atlanta Hospital, my director approached me several weeks ago to put together a crisis plan for my team and several of the cardiac service lines. The main focus for developing the plan was to decrease the APPs’ exposure to and risk of acquiring COVID-19. Following implementation, I wanted to share several tips regarding crisis planning plus some important lessons learned along the way.
Dividing into teams
Our APPs work 4- to 10-hour shifts divided up over seven days. I combined the advanced heart failure team, the heart valve team, electrophysicology (EP) team, and the general cardiology team into one large group. I divided them into three teams with one to two representatives from each sub-speciality on each team. By spreading out the sub-specialty APPs, we can continue to provide specialized cardiac care regardless of the team.
I changed the work schedule to four days on and seven days off, alternating with three days on and seven days off (4:7, 3:7). One team works while two teams are recouping with decreased exposure; nine to ten APPs work while 18 to 20 are actively decreasing their exposure. Overall, the APPs are reducing their exposure by 12.5%: 14 days, 10 hours, 14, 1 day, 14. We have contingency plans for any reductions in the teams as the surge occurs.
Tips for Developing a Crisis Plan
Develop a way to communicate with your teams. I have a total of six teams including the night team. Some of the information shared is appropriate for all the teams but some is very specific to only one team. During a crisis, information is shared quickly and you need to convey this to 50-plus APPs in a timely, concise and succinct manner. The sooner you learn the best ways to communicate with your teams, the more agile your people will become.
Be transparent. When you think you have been transparent, challenge yourself to become even more so. During a crisis your team looks to you for guidance, information, and safety. There is no better way to convey this than sharing timely information and being transparent, not only with current topics but also with expectations for the next seven to 10 days.
Get stakeholder input. A required class for my iMBA program is Managing Organizations during which we discussed change management. This new schedule at the Piedmont Heart Institute is a complete change from normal. Include your APPs on the front end of crisis planning, development and implementation. It will pay huge dividends when it goes into effect. When people are included in planning change, they are much more likely to adopt it and fight to make it work.
Do not ask someone to do something that you wouldn’t. The first day our team was going to see COVID-19 positive patients I was on call and requested to have all of them assigned to me. By leading from the front, I was able to model the behavior that I wanted and expected from my teams. I have not had an APP refuse to see a patient.
Be unified with your leadership. In times of high stress and crisis people become very sensitive to any variation in what they are being told. Make sure that you are checking in with your leadership once or twice daily so that you can be on top of any changes to policies, or new policies, that are coming out. The director and I have a phone call “sign-in” every morning and a phone call “sign-out” every evening, so that he is aware of anything going on with the teams and I am aware of any changes from top leadership.
Be an advocate for your teams. Advocate whether in meetings, to other leaders/managers, to other medicine teams, or by getting out ahead of your teams in order to protect them. As leaders, our most important responsibility is to the people we lead.

Lessons learned
In addition to planning and implementation tips, I also learned several important lessons around crisis planning.
First, people don’t want time off. Of course, people do want time off; it is one of the most important benefits people look for in new positions. During our crisis time all PTO/CME has been suspended, but the schedule gives APPs seven days off between shifts. APPs tell me they were “going crazy” at home for that long. One APP was transitioning to a new team and was going to be off for 10 days; they requested to start working earlier.
Stepping up and bonding
Not only are they taking less time off, but APPs have stepped up without question, even the inflexible, non-volunteering sorts. This is not a surprise or shock since we all got into medicine to help people. A pandemic kicks these feelings into overdrive. APPs have changed their schedules, canceled their vacations, and found creative ways for childcare so that they could be here caring for patients.
During times of crisis team bonding is accelerated. This is a phenomenon the military has recognized for years. However, to see it is to believe it. We grouped four different service lines, including APPs who never cross paths and wouldn’t call each other for simple things. They are now celebrating birthdays together, covering each other so that people can leave early, sharing scarce resources, and talking about having family outings after the crisis passes. The deep, rapid bonding has been interesting to see and fantastic for morale.
Good leaders will be recognized
It goes without saying that you cannot please everyone. When altering over 50 APPs’ personal and professional lives, you hope to accommodate people as best you can. Unfortunately, “you cannot please everyone” has been reinforced for me several times since this change was implemented. Be as fair as possible and when someone looks back on your decision in six months it should be clear to them that it was fair, equitable and consistent among all the team members.
People appreciate leaders looking out for them. I continue to be surprised, happily, from the outpouring of appreciation for the crisis planning, scheduling, transparency, fairness, and “all that you do”. In the iMBA program I took a class called Leadership and Teams and we discussed that leaders’ major responsibility is to the people they lead. Good leaders will always be recognized by their teams.
Kyle Fortman, PA-C, graduated from Cook County Hospital/MXC PA Program. He received his MPAS degree from University of Nebraska Medical Center and will earn his MBA from University of Illinois at Urbana-Champaign (iMBA) in December. Contact him at [email protected].
You May Also Like
Rush University PAs Integral to Coronavirus Response
Not on the Front Lines? Ways You Can Help With COVID-19 Response
PA Resources for COVID-19; Share Your Story with Us
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



