Rush University PAs Integral to Coronavirus Response
Director of APPs Jennifer Orozco, MMS, PA-C, DFAAPA, Coordinating Effort
March 13, 2020
By Eileen Denne, CAE, APR
Across the country, PAs and other healthcare providers are stepping up to address coronavirus, COVID-19, as daily reports surface on new cases.

On March 11, the World Health Organization declared that the global coronavirus is now a pandemic. In Illinois, which reached a total of 25 cases on March 12, PAs are a vital part of Rush University Medical Center’s response efforts, which include maximizing telemedicine and executing an emergency surge code to ensure more beds are available. Jennifer M. Orozco, MMS, PA-C, DFAAPA, director-at-large on AAPA’s Board of Directors and co-director of Advanced Practice Providers (APPs) in the Office of Advanced Practice (OAP) at Rush, is right in the thick of it.
In her role as director of APPs, including PAs and APRNs, Orozco is part of the leadership team in the command center at Rush. There are almost 50 people on the senior team including C-suite members like the CEO, chief medical officer, and chief operating officer, as well as other key directors or senior vice presidents associated with nursing, medical staff, and hospital operations.
“Rush has a very APP-positive culture,” said Orozco. “We are valued members of the healthcare team and since appreciation for what we do is already part of the Rush culture, it’s made the coronavirus mobilization even more effective.”
Training and mobilizing APPs
“We are currently training and mobilizing teams of APPs to help with the influx of patient care,” Orozco says. “PAs and NPs are conducting video visits and e-visits with patients who have common illnesses including concerns for coronavirus; APPs are among the providers staffing a new clinic that will only be used to test patients for possible coronavirus. We will also use them during the patient surge whereby NPs, PAs and physicians will staff new patient care units all over campus.”
There are nearly 400 APPs at Rush with 27 Lead APPs who help manage teams of APPs and day-to-day clinical operations. Orozco also has a team in the OAP that helps lead and organize important projects; collects APP specific data; and coordinates orientation, onboarding, and professional development.
Orozco says the Rush ambulatory transformation team and information systems team created a digital platform to enable patient access to a physician or APP via electronic visits. Any new or returning patient can download the Rush mobile app, log in and request to see a provider to treat any common illness such as a cough, runny nose, pain with urination, etc.
“This allows us to keep these types of patients out of our emergency room (ER) and allows them to receive care at home. Recently, we expanded this platform to video visits so that patients can have face-to-face visit with a provider (physician or APP) to discuss their concerns,” Orozco says.
Telemedicine allowing for greater access to patients
Telemedicine shows promise for treating infectious disease such as coronavirus because one of the goals with COVID-19 is to prevent community spread. Hospitals like Rush want to keep people with possible symptoms out of the ER and clinics to decrease the chances of infecting other people.
“Telemedicine allows us to mobilize large teams of APPs and physicians to talk to patients and control how we test them by minimizing possible spread to others,” Orozco says. “We are continuing to build our telemedicine platform and recently expanded to video visits. About 10 days ago we began offering coronavirus screenings via our virtual platform and the response has been overwhelming.”
Rush’s other recent actions to respond to COVID-19 patients included a decision to execute an emergency surge code and add beds in places where they don’t normally have them.
“We’re doing emergency credentialing and privileging of APPs to help us,” Orozco says. “We’re opening up a number of beds staffed by APPs this week. We have asked for volunteers and met with APP leadership to ask whom they can clear with their team. We’re have had almost 200 APPs volunteer, especially for telemedicine.”
“It has been pretty amazing to me how providers at Rush can drop everything and come together to volunteer to provide patient care outside normal hours and across the organization. These volunteers don’t ask about compensation; they just want to know what they can do.”
Hospital bylaws and state law are barriers to APP response
Hospital bylaws and state law have impacted Rush’s ability to maximize APP practice in response to the virus. Orozco says the good news is that in Illinois, APPs don’t have to have collaborating physicians on file with the state in the hospital setting, but hospital medical staff bylaws and insurance carriers require it. In their efforts to mobilize, Orozco says, they have had to urgently identify collaborating physicians, which adds an extra layer of work.
Rush is also opening up new beds to accommodate an influx of patients. By state law, patients can only be admitted by a member of the medical staff; APPs are not officially members of medical staff. APPs still have to be tied legally to a physician to ostensibly provide oversight even through the APPs are providing care.
“These unnecessary administrative burdens get in the way of patient care, which is a big reason why we are advocating to modernize not only hospital bylaws but state law as well,” said Orozco.
Advice for other APP directors
Asked about advice she would give to other APP directors, Orozco says they need to start thinking about their team flexibility across the organization.
“This past week has been critical to get prepared at Rush. We’re just trying to be ready to go so we can continue with business as usual. Consider what administrative barriers and what state barriers to address if you do have an influx of patients and think about how you will be able to deploy APPs to inpatient, ambulatory and telemedicine patients. Figure it out now so you’re not doing everything at the last minute and don’t have proper paperwork. Be creative.”
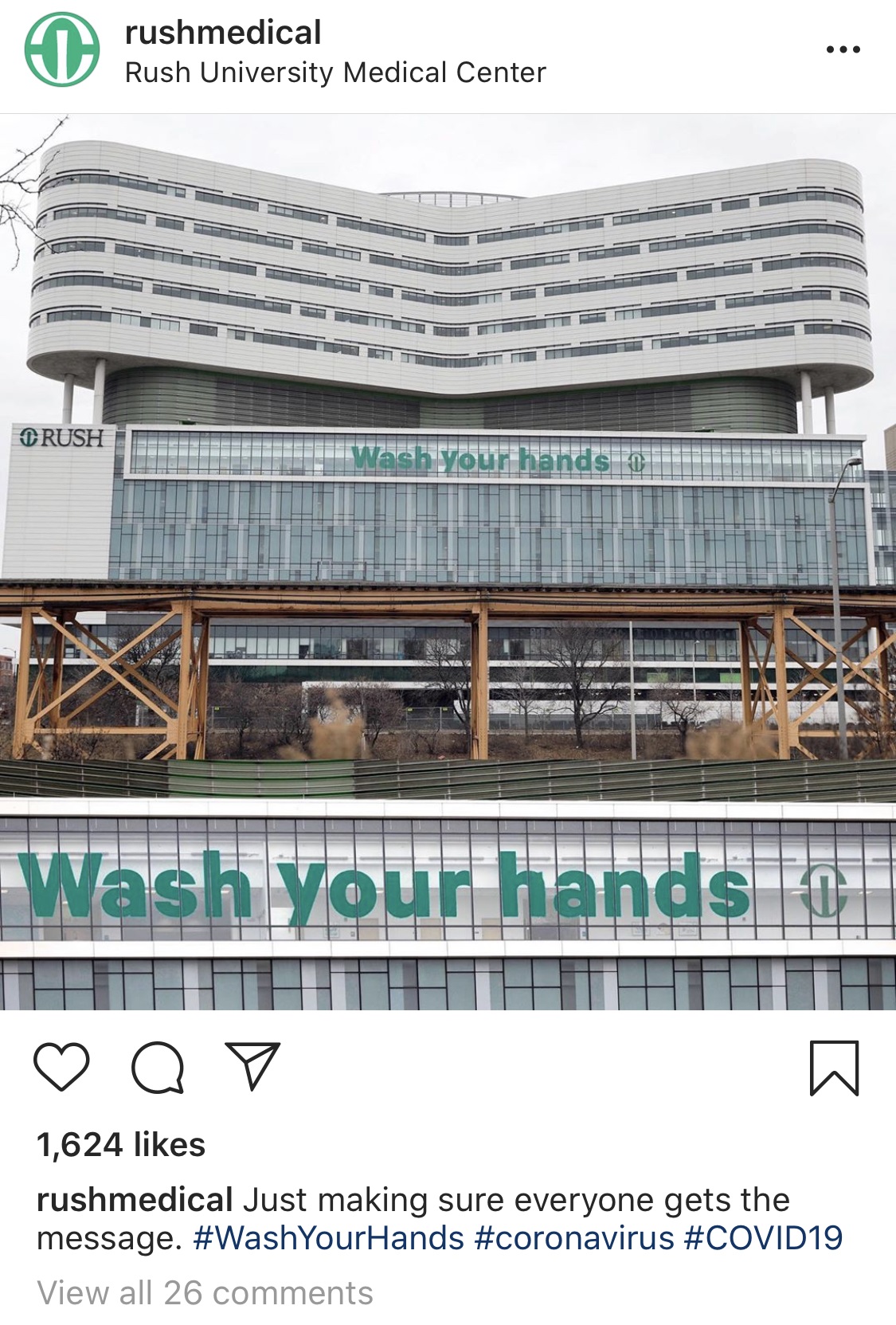
Orozco’s advice to all PAs during the COVID-19 crisis is to keep calm, stay informed, and wash their hands. The CDC COVID-19 guidelines are updated daily, sometimes several times a day, so providers can inform patients who are nervous.
Eileen Denne is director of Corporate Communications at AAPA. Contact her at [email protected].
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



