Health Inequities: How PAs Can Help Bridge the Care Gap
Listen to Vital Minds Podcast Episode
July 2, 2021
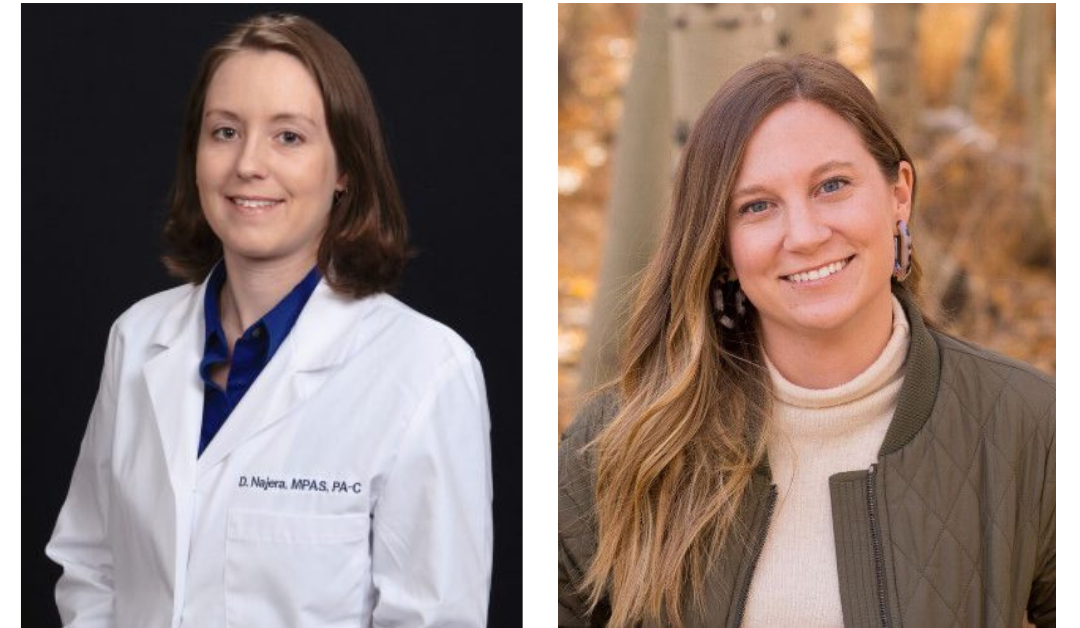 The PA Foundation’s Vital Minds podcast recently featured a discussion on how health disparities have been exacerbated by the COVID-19 pandemic, the role that socioeconomic factors and insurance may play in health disparities, and how PAs – and other allies – can help bridge the care gap. This episode featured a conversation between Deanna Bridge Najera, PA-C, DFAAPA, who practices in emergency medicine and serves as a clinician consultant in Carroll County, Maryland, and Tori Marsh, MPH, director of research at GoodRx, a company which provides a range of services to help people get the healthcare they need at a price they can afford. Andrea Lowe, MBA, MHA, PA-C, AAPA’s director of employer strategy and diversity, equity, and inclusion business partner, led the discussion.
The PA Foundation’s Vital Minds podcast recently featured a discussion on how health disparities have been exacerbated by the COVID-19 pandemic, the role that socioeconomic factors and insurance may play in health disparities, and how PAs – and other allies – can help bridge the care gap. This episode featured a conversation between Deanna Bridge Najera, PA-C, DFAAPA, who practices in emergency medicine and serves as a clinician consultant in Carroll County, Maryland, and Tori Marsh, MPH, director of research at GoodRx, a company which provides a range of services to help people get the healthcare they need at a price they can afford. Andrea Lowe, MBA, MHA, PA-C, AAPA’s director of employer strategy and diversity, equity, and inclusion business partner, led the discussion.
COVID-19 has exacerbated health inequities
“Health equity is the concept that calls on us as healthcare providers to bridge the gaps that lead to disproportionate incidences of all issues, from COVID-19 to chronic disease,” Najera explains. She and Marsh agree – as does the data – that COVID-19 disproportionately affects communities of color, resulting in health inequity. “COVID-19 is really affecting communities of color to a greater degree,” Marsh affirms. “The death rate is higher for Black and Hispanic individuals,” she continues, citing the CDC’s statistics, “and [GoodRx’s] research shows that communities of color tend to have fewer pharmacies per capita, which puts [these communities] at a disadvantage in the COVID-19 vaccination efforts.” Areas with limited access to pharmacies are called pharmacy deserts, and Marsh says these pharmacy deserts could lead to vaccine deserts, areas “where the rate of vaccination is lower, simply because there aren’t enough appointments available.”
[Help support the PA Foundation]
Socioeconomic circumstances and insurance coverage impact patient care
While the pandemic has exacerbated issues of health inequity, these gaps would still exist without COVID-19. A family or individual’s insurance coverage – or lack thereof – and income level can affect how they seek out both preventative care and emergency resources. Najera recalls how emergency visits increased when the Affordable Care Act passed because “individuals finally had health insurance but did not have access to the actual providers to care for their needs. They would come to the emergency department (ED) with what we consider non-emergent complaints,” she says, “because they couldn’t afford to take a day off work to see their primary care provider for preventative care.”
“Even when patients have insurance, they’re often still limited in their ability to see a primary care provider,” Najera continues. “Some primary care providers are limited in the number of patients they can see who have state or federal insurance because the reimbursement rates are so low. Or their insurance plans have very high deductibles, so they put things off until it’s a catastrophic event.” As a PA in the ED, Najera makes it a priority to help solve problems and connect patients with the treatment they need.
Marsh’s research corroborates Najera’s observations. “GoodRx is consistently tracking prescription affordability,” she notes. According to GoodRx’s survey of over 1,000 Americans of all ages and genders, one-third of respondents said they have skipped filling a prescription one or more times simply because of cost. “These skipped prescriptions can lead to complications for untreated conditions and increase healthcare costs overall – increased hospitalizations, surgeries, or emergency medical care,” Marsh explains. GoodRx’s research shows that insurance plans are not only covering fewer and fewer drugs, but more restrictions are also being placed on patients. For many patients, an increase in the number of prior authorizations and/or specialist visits needed, as well as an increase in the patient’s share of costs (i.e. copays and deductibles), is making needed prescription drugs unaffordable. These systematic issues contribute to ongoing health inequities.
[More from Deanna Bridge Najera: Learn How Implicit and Overt Bias Impact How You Practice]
PAs have an opportunity to be allies
Given the increased awareness of health inequities, Najera and Marsh view the current environment as an opportunity for PAs to be allies. “PAs can meet patients where they are,” Marsh advises. “Whether they are experiencing homelessness, whether they are unable to afford their medications, whether they are uncomfortable using their insurance – PAs are perfectly suited to have these conversations. Initiate that open dialogue.”
“I always make sure I’m hearing what [the patient] is saying and maybe also what they’re not saying,” Najera shares. In addition to these open conversations with patients, she also recommends that healthcare providers have a better understanding of their own privileges and biases. “Don’t be afraid to question your opinions and examine how you’ve interacted with people different from you in the past. [Use] good and bad [interactions] as learning experiences, and then create better interactions going forward.”
You May Also Like
Vital Minds Podcast
PA Foundation
Diversity, Equity, and Inclusion Webinar Series
Learn How Implicit and Overt Bias Impact How You Practice
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.