What PA Practice Looks Like in Neuro-Oncology
Patient Population Requires Preparation, Practice, and Patience
June 28, 2024
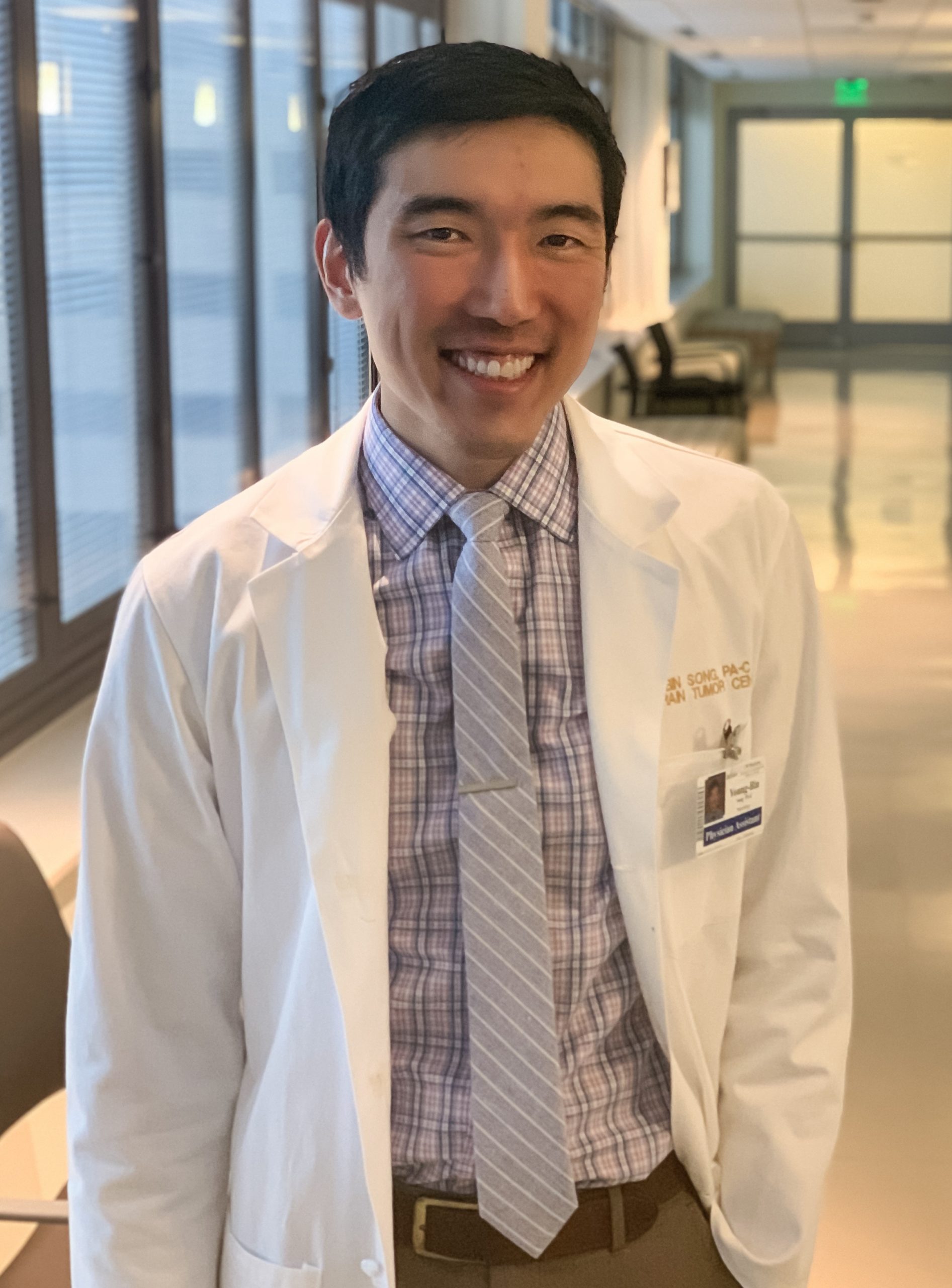
By Young-Bin Song, MCHS, PA-C
I became interested in becoming a PA after meeting a surgical PA while working at Children’s of Alabama. I journeyed from Birmingham, Alabama, to the Pacific Northwest, where I attended MEDEX Northwest PA Program at the University of Washington. I was initially interested in many different specialties, but after reading Atul Gawande’s “Being Mortal: Medicine and What Matters in the End,” I clearly knew that I wanted to work with the oncology population. I accepted a position at a multi-disciplinary neuro-oncology/radiation oncology brain tumor clinic, and I recently celebrated my four-year anniversary at the clinic.
Neuro-oncology and radiation oncology
I am privileged to work with a group of physicians who are expert in central nervous system (CNS) cancers, including gliomas (glioblastoma, oligodendroglioma), meningiomas, primary CNS lymphomas, spinal cord tumors, and brain and leptomeningeal metastasis. Our radiation oncologists use different radiation tools to treat CNS cancers by determining planning/delivery modality, determining a target volume and creating an individualized treatment plan (i.e. fractionated, stereotactic radiosurgery, whole brain radiation therapy, photon vs proto). Our neuro-oncologists combine their expertise in both neurology and oncology to deliver therapies (such as chemotherapy, immunotherapy, Optune device), manage neurologic side effects and complications, and navigate active surveillance, tumor survivorship, and end-of-life/hospice care.
I work with two other advanced practice providers (APPs) in the clinic and work closely with our neurosurgical colleagues, neuro-radiologists, neuro-pathologist, and Fred Hutchinson Cancer Research Center oncology groups, when we all meet weekly for a tumor board conference.
[A Day in the Life: How PAs Practice]
Brain tumor clinic
I work in an outpatient clinic. Each patient is assigned an MD, APP, and an RN, and we work as a team to accomplish each goal. I often see new visits with a neuro-oncologist and/or radiation oncologist, where we discuss the diagnosis and treatment options and plans. Then I see patients at various points during their treatment and surveillance. I help and prepare chemotherapy orders and manage its toxicities, complications, and side effects, such as neutropenia, thrombocytopenia, deep vein thrombosis, and immunotherapy toxicities (NCCN has many guidelines on chemotherapy and immunotherapy managements). I also perform Ommaya reservoir taps and therapeutic intrathecal injections.
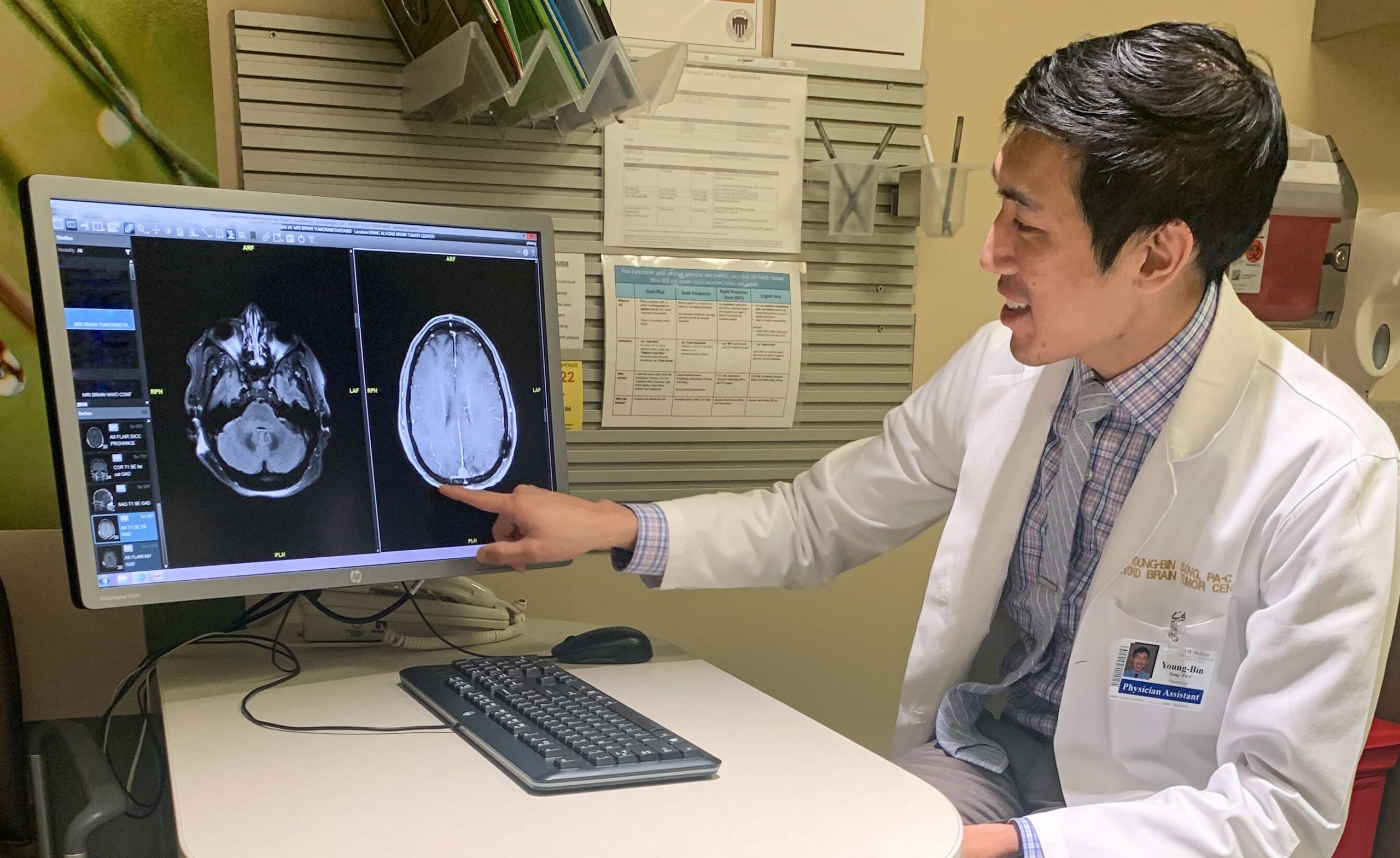
I also manage many neurologic complications, such as seizures, headache/pain, cerebral edema, weakness and numbness, and cognitive and mood issues. Like other various neurologic conditions, including multiple sclerosis, stroke, and Parkinson’s disease, our patients often have many physical, occupational, and speech-language deficits, and we work closely with our social worker and the neuro-rehab team. During visits with a new MRI study, I read and interpret the images and go over it with patients and families. Learning to read and interpret many different MRI brain sequences has been a huge learning curve and I’m thankful that I have my attending and neuro-radiologist available to review them. When I am not seeing patients, I work with nurses to triage symptom calls, refill medications, and order labs.
[Seattle Cancer Care Alliance APPs Focus on Collaborative Approach]
Palliative care
Brain tumor diagnosis is often devastating and unexpected, and our patients face unique challenges due to neurocognitive, neurobehavioral, and quality-of-life issues. These challenges require palliative care skills and I use palliative care communication tools to help navigate different challenges and obstacles, such as breaking bad news, addressing conflicts and emotions, and end-of-life discussions. I also engage in goals of care discussions, assess activity of daily living and quality of life, and provide education to patients and family members. These communication skills are invaluable to our patient population and require lots of preparation, practice, and patience. I am fortunate to learn these skills from two of our neuro-oncologists who also are board-certified in palliative care. Also, there are fantastic resources from the VitalTalk website with example videos and a VitalTips app, which I use as a refresher and a quick resource before going into clinic visits. It is so rewarding when I get to be part of this hard work that brings patient-centered care, empathy, and dignity to patients and family caregivers.
Never stop learning
Even after being here in the clinic for four years, I feel like I’ve only scratched the surface. The field of neuro-oncology is a marathon, not a sprint, and it is also changing faster than ever, with many current and future clinical trials using novel approaches. I am continually trying to learn more, whether in tumor board discussions or being more proficient in neuroanatomy. Each of our APPs brings their unique practice backgrounds and I’m lucky to learn from them as well. In addition, one of the best ways to retain what I’ve seen (“see one”) and acquired (“do one”) is to “teach one,” so it’s been a rewarding experience to return to my PA school to help out with neuro exams. Most importantly, I have learned so much from my patients and families and I am so grateful and honored to be part of their journey.
Originally published February 19, 2020.
You May Also Like
PAs in Hospice and Palliative Care
Seattle Cancer Care Alliance APPs Focus on Collaborative Care
A Day in the Life: How PAs Practice
Young-Bin Song, MCHS, PA-C, is a PA and teaching assistant at Alvord Brain Tumor Center, UW Medicine, Department of Neurology, University of Washington School of Medicine. Contact him at [email protected].
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



