Maine PA Experienced Challenges in Pursuit to Provide Psychiatric Care
October 3, 2018
The number of mental healthcare providers in Maine only meets the needs of roughly one-third of the population. Yet, when a PA in Maine — who had recently completed a Veteran’s Administration residency program in psychiatry — sought a job in the Bangor area, he faced many hurdles due to outdated state laws.
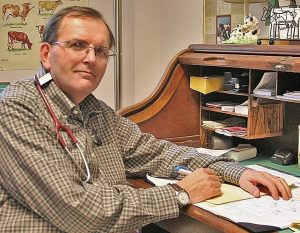
PA Dana Green practiced nearly 20 years in primary care and internal medicine specialties. However, when a health set-back severely affected his ability to practice in these specialties, he took full advantage of the flexibility of the PA profession and decided to continue his career in an area of patient need – psychiatry. Prior to even starting the residency program in psychiatry, he was thrilled to have identified a psychiatrist at a nearby hospital who said he would be happy to have Green come on board after he completed his residency.
However, upon returning to Maine, Green discovered the hospital policy was to only hire NPs with psychiatry training. This is not uncommon in Maine, even though, according to the Center for Medicare and Medicaid Services, “PAs are trained on a medical model that is similar in content, if not duration, to that of physicians. Further, PA training and education is comparable in many ways to that of APRNs, and in some ways, more extensive.” Unfortunately, state laws governing PA-practice require PA-physician teams to adhere to certain requirements including face-to-face meetings and chart reviews that aren’t required of NPs. This causes employers to perceive that hiring PAs comes with administrative burdens not required for NPs.
“I’ve always appreciated having that physician-PA relationship, but there are definitely situations and settings where physicians and PAs need more flexibility. It’s time for Maine to review PA-practice laws and better align them with the needs of our patient population,” said Green.
Thankfully, Green was offered a temporary position at the local VA in outpatient psychiatry. The position enables him to meet with and care for patients affected by substance use, bipolar or psychotic disorders, and more. He’s worked with countless patients who have nowhere else to turn—a continual reminder of how critical it is to have access to psychiatric care. Unfortunately, his temporary position at the clinic might soon be at stake. The VA hired a new psychiatrist who will start seeing many of Green’s current patients. As a result, Green is considering a part-time position at a hospital 125 miles away so that he can continue using his new skills to help patients in need.
The need for mental healthcare providers in Maine remains, but Green and other PAs in the state will continue to run into challenges when securing jobs in mental health.
When PAs, physicians, and other medical professionals can work together to provide quality care without burdensome administrative constraints, they can achieve Optimal Team Practice. However, to achieve this, Maine must modernize laws and regulations affecting PA practice. This will strengthen healthcare teams, expand access to care, reduce healthcare costs, and enable those like PA Green the flexibility to use their skills to the fullest extent.
Find out how PAs can contribute to Optimal Team Practice.
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



