Outdated Laws Threaten Future of Patient Care in Rural Oregon
November 9, 2017
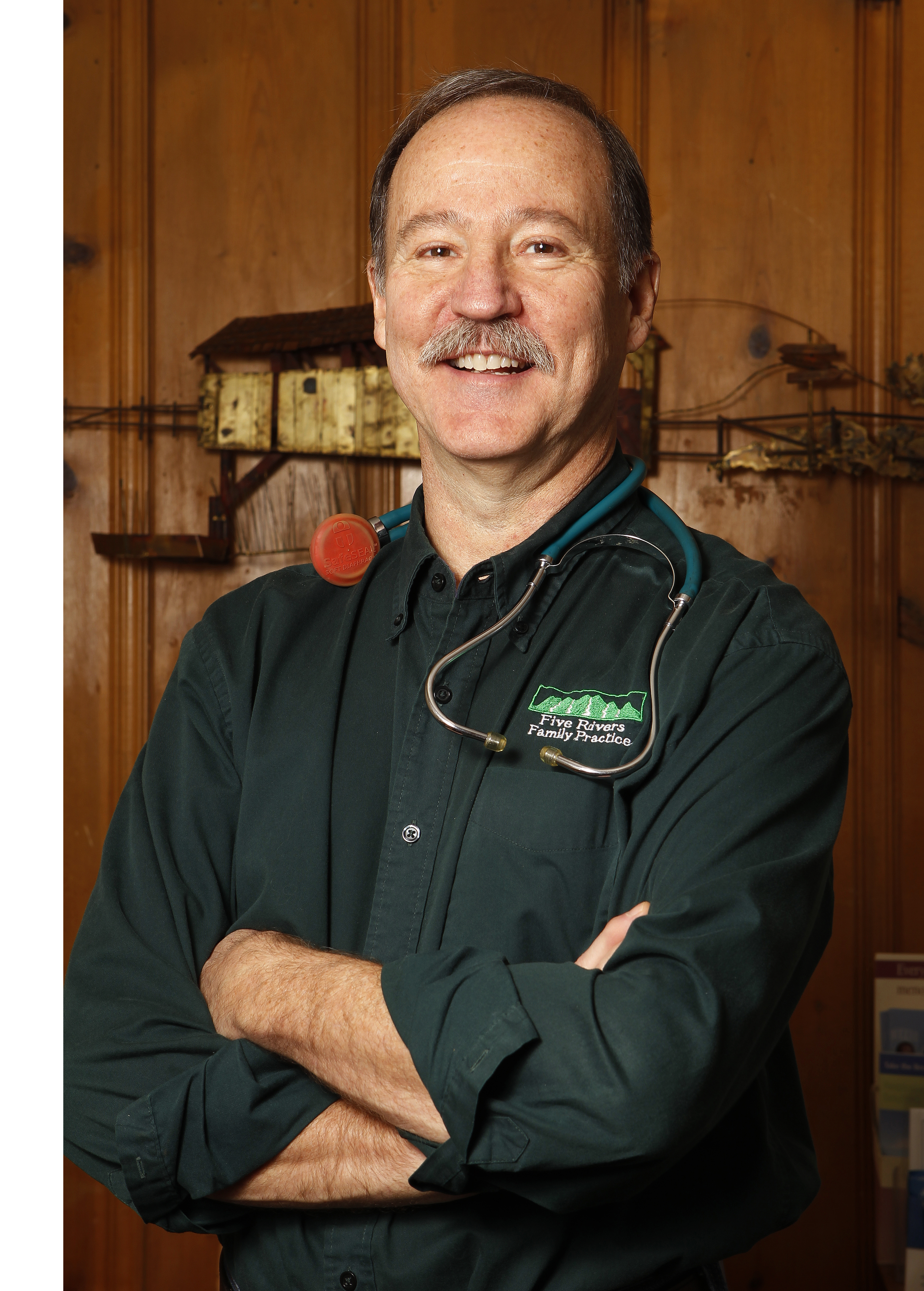
Across the U.S., many people who live in rural areas struggle with access to quality, affordable healthcare. Edwin Weih, PA-C, knows this challenge well as he practices in Oakridge, Oregon, a town with only 3,500 residents.
For two decades, PA Weih’s primary care clinic has been a reliable presence in the community, providing medical care to patients who would otherwise have to travel great distances to receive—or simply go without. Unfortunately, outdated PA practice laws are threatening patients’ access to care in Oakridge as well as Weih’s ability to practice.
Today, Oregon and all other states require PAs to have a supervisory or collaborating agreement with a physician in order to practice. Some state laws and regulations go into even more detail as to what is required at the practice level.
For example, in Oregon, the physician with whom Weih practices must review a certain percentage of Edwin’s patient charts. One day per month, the physician must also travel to Oakridge, which is over an hour away from his primary practice location.
“These requirements are an administrative hassle that have no impact on patient care,” said Weih, who is growing increasingly concerned about what happens to the patients he serves once the physician he works with retires. The rural physician workforce is aging. If Weih can’t find another physician willing to enter into a supervisory agreement with him, he may have to close his practice.
Also, the healthcare marketplace has changed—not only in Oregon but across the country. As more and more physicians are employees rather than practice owners, the incentives for physicians to supervise PAs have diminished. Physicians also increasingly don’t want to assume PA supervision liability.
When PAs, physicians, and other medical professionals can work together to provide quality care without burdensome administrative constraints, they can achieve Optimal Team Practice. One way to achieve this is to remove the requirement for PAs to have an agreement with a specific physician. This will strengthen healthcare teams, expand access to care, reduce healthcare costs, and enable those like PA Weih to continue providing high-quality care to their patients, regardless of whether they have a formal agreement with a specific physician.
“It’s just clear that the laws and regulations that were put in place decades ago must be changed to meet modern healthcare needs,” said Weih, who added, “I depend on physicians every day, and have great respect for the depth of physician training. I wouldn’t think of practicing without physician input.”
Find out how PAs can contribute to Optimal Team Practice.
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



