What Barriers Stand Between PAs and Rural Settings, MUAs, and HPSAs?
Opportunities for spouses, compensation, and scope of practice lead the list
October 12, 2022
By AAPA Research
Approximately half of the PAs who responded to the 2021 PA Practice Survey were either already working in, or were interested practicing in, a rural location, medically underserved area (MUA), or health professional shortage area (HPSA). However, recruiting new providers to these areas and encouraging them to remain can be challenging. In a few demonstration projects, when NPs have been granted full practice authority, a greater proportion of NPs have moved into rural areas. Even when the majority of the NPs have moved to urban areas, there is still a significant increase in access to care for patients in rural locations1-5. Communities also benefit economically when PAs move to work in rural locations6.
To learn more about the pathway to practicing in rural locations, MUAs, and HPSAs, we gathered information on barriers and the demographics of interested PAs, and PA students, and reported our findings in the data brief PA Interest in Rural Locations, Medically Underserved Areas, and Health Professional Shortage Areas: Review & Recommendations.
PA Interest varies by career stage
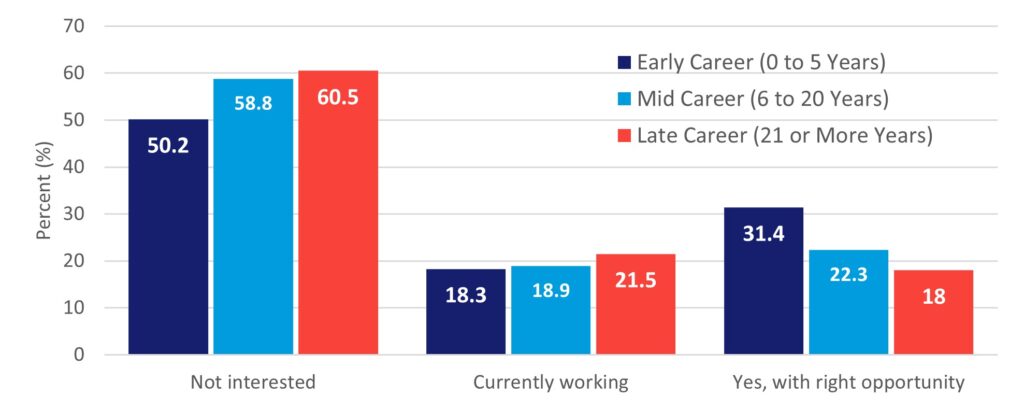
A PA’s career length and specialty had an impact on their desire to work in rural locations, MUAs, or HPSAs. For example, while 44% of all PA respondents in the 2021 PAPrS survey were either interested or already working in rural locations, this interest varied by how long they had been practicing as a PA. Figure 1 illustrates how early career PAs are less likely to be currently working in rural locations; however, they are also the group most interested in future rural practice if given the right opportunity. Within our data brief, we also discuss the role PA specialty plays in a willingness to work in rural areas. PAs in pediatrics were the least interested while those in emergency medicine were the most likely to be working in rural locations or open to working in these areas if given the right opportunity.
Figure 1. Interest in Rural Locations by Career Experience
Lack of Spouse opportunities rated the most severe barrier to PA practice in rural locations and MUAs/HPSAS
Four factors were rated as a moderate or severe barrier to practicing in rural locations or/and MUA/HPSA. The rankings were similar between the two categories, but there were some key differences. Not having career opportunities for a spouse/partner was the top barrier to working in a rural location or an MUA/HPSA, but the perceived severity of this barrier was greater in rural locations (74%) than MUAs/HPSAs (66%). Conversely, compensation was a larger barrier to MUA/HPSA practice (59%) than practicing in a rural location (57%).
Where a PA student grew up is related to their interest in rural practice
In the 2022 AAPA Student Survey, we asked PA students about their future interest working in rural locations, MUAs, and HPSAs with the question “Which of the following settings do you have an interest practicing in at some time in your career?” In general, 54% of students were interested in rural locations and 70% were interested in MUAs and HPSAs. However, interest varied when we examined how the responses from students who grew up in towns with a population of 10,000 or less compared to those from more urban areas. These figures are presented in Table 1. While students from urban areas and their small town/rural classmates had similar interest in MUAs and HPSAS, their ranking of rural locations was very different. Only 47% of students from more urban areas were interested in rural locations while 74% of those from small towns and rural areas are interested working in this setting at some point in their career. These findings echo the work from the WWAMI Rural Health Research Center7-8.
Table 1. PA Student Interest in Working in Rural Locations, Medically Underserved Areas and/or Health Provider Shortage Areas, and Working with the National Health Service Corps in 2022 by the Community They Grew Up in
| Location | Urban areas a | Small town and rural areas b | ||
| N | Percent (%) | N | Percent (%) | |
| Medically Underserved Area/HPSA | 1,476 | 71.5 | 505 | 72.2 |
| Rural Location | 1,003 | 47.2 | 515 | 73.7 |
| National Health Service Corps | 568 | 26.8 | 214 | 30.6 |
| None of the above | 319 | 15.0 | 47 | 6.7 |
Source: 2022 AAPA Student Survey.
Question: Which of the following settings do you have an interest practicing in at some time in your career?
Question: What is the type of geographic area where you were raised?
If you had multiple childhood homes, please answer in terms of a majority of your childhood. Respondents could answer: Urban (population 1,000,000+), Large city (population 100,000 to 1,000,000), Mid-size city (population 50,000 to 99,999), Large town (population 10,000 to 49,999), Small town (population 2,500 to 9,999), Isolated rural (population <2,500), or Military or government installation.
Notes: a. Urban areas (estimated population of 10,000 or more) is Urban (population 1,000,000+) to Large town (population 10,000 to 49,999). b. Small town and rural areas (estimated population of less than 10,000) is Small town (population 2,500 to 9,999) and Isolated rural (population <2,500). c. Military or government installation was excluded from this analysis. d. Respondents were allowed to make multiple selections, totals do not add to 100% and instead represent the proportion of respondents who selected the response category.
This article was written by Sean Kolhoff, Ph.D., Senior Research Analyst at AAPA. Contact him at [email protected].
You May Also Like
PA Interest in Rural Locations, Medically Underserved Areas, and Health Professional Shortage Areas: Review & Recommendations
Physician assistants in rural communities (JAAPA)
Updating PA Practice Laws May Improve Rural Healthcare Access
Two Fellowship Awards Available for Preceptors Serving Underserved Populations
References
- Barnes H, Richards MR, McHugh MD, Martsolf G. Rural And Nonrural Primary Care Physician Practices Increasingly Rely On Nurse Practitioners. Health Aff (Millwood). 2018;37(6):908-914. doi:10.1377/hlthaff.2017.1158
- Holmes LR, Waltman N. Increased access to nurse practitioner care in rural Nebraska after removal of required integrated practice agreement. J Am Assoc Nurse Pract. 2019;31(5):288-292. doi:10.1097/JXX.0000000000000153
- Neff DF, Yoon SH, Steiner RL, et al. The impact of nurse practitioner regulations on population access to care. Nurs Outlook. 2018;66(4):379-385. doi:10.1016/j.outlook.2018.03.001
- Patel EY, Petermann V, Mark BA. Does State-Level Nurse Practitioner Scope-of-Practice Policy Affect Access to Care?. West J Nurs Res. 2019;41(4):488-518. doi:10.1177/0193945918795168
- Young SG, Gruca TS, Nelson GC. Impact of nonphysician providers on spatial accessibility to primary care in Iowa. Health Serv Res. 2020;55(3):476-485. doi:10.1111/1475-6773.13280
- Eilrich FC. The economic effect of a physician assistant or nurse practitioner in rural America. JAAPA. 2016;29(10):44-48. doi:10.1097/01.JAA.0000496956.02958.dd
- Larson EH, Andrilla CHA, Morrison C, Ostergard S, Glicken A. (2016). Which Physician Assistant Training Programs Produce Rural PAs? A National Study. WWAMI Policy Brief #154. Retrieved from: https://depts.washington.edu/fammed/rhrc/wp-content/uploads/sites/4/2016/02/RHRC_PB154_Larson.pdf
- Larson EH, Coulthard C, Andrilla CHA (2018). What Makes Physician Assistant (PA) Training Programs Successful at Training Rural PAs? WWAMI Policy Brief #164. Retrieved from: https://depts.washington.edu/fammed/rhrc/wp-content/uploads/sites/4/2018/06/RHRC_PB164_Larson.pdf
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



