With State-of-the-Art Facilities and Full-Tuition Scholarships, Chapman University Trains PAs to Meet Need for More Primary Health Care Providers
January 14, 2022
SPONSORED

Across the United States, there is a shortage of primary care providers. Chapman University is at the forefront of a vital response to the challenge – preparing PAs.
“PAs are the future of healthcare in the United States,” says Michael Burney, director of Chapman’s PA Program. “PAs provide skilled, cost-effective care that helps take the pressure off a strained system.”
Educating PAs is a crucial step toward meeting the demand for healthcare, says Janeen Hill, Ph.D., dean of Chapman’s Crean College of Health and Behavioral Sciences, where the PA program is located.
“Investing in the training of PAs and other healthcare professionals is the best way to meet an increasing need for primary care,” Hill says. “It’s faster and more effective to prepare a new generation of PAs.”
Chapman’s Crean College is home to a growing PA Program, which in 2018 graduated its first class of 25 practicing PAs.
Commitment to Support for Underserved Students
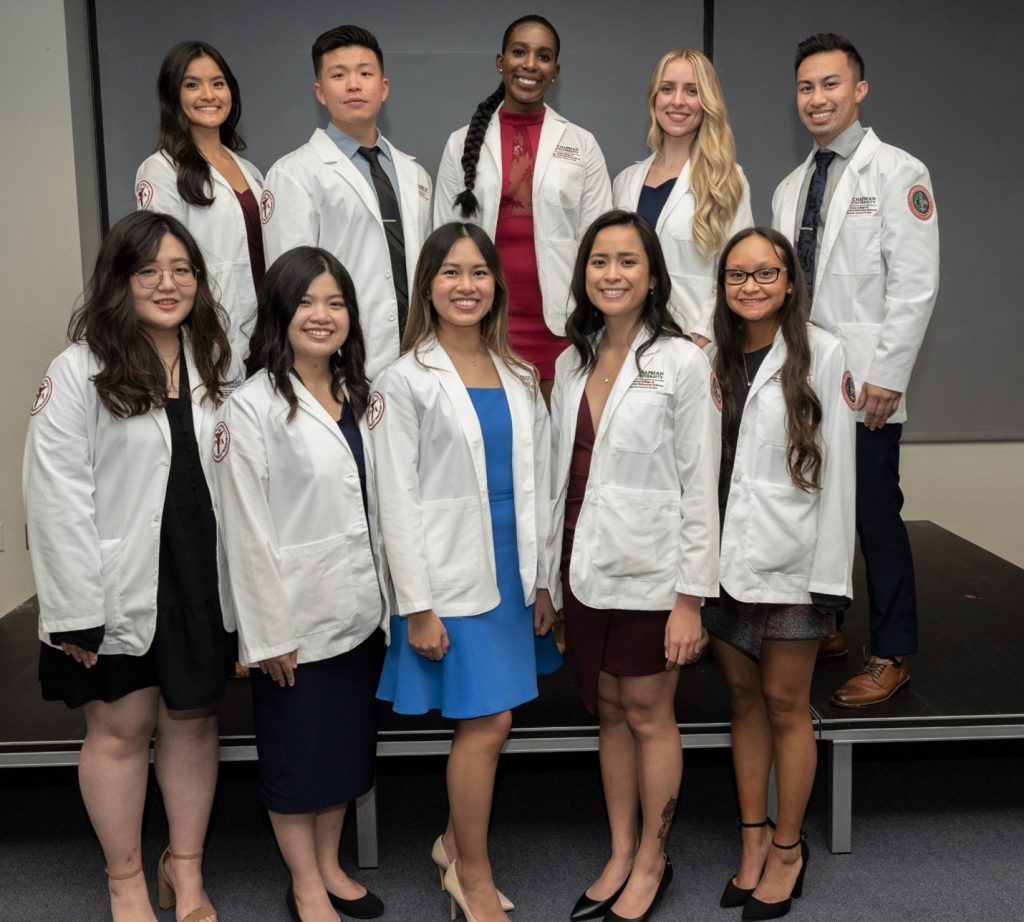
Since then, the program has expanded and now offers full-tuition scholarships to qualifying students. Building on its dedication to helping underserved students pursue higher education, the Simon Family Foundation donated $9 million to support the Simon Scholar PA Program. Ten full-tuition scholarships are provided each year to students who want to earn their Master’s in Medical Science (MMS) in Chapman’s PA program. Each scholarship awardee commits to practicing clinically in underserved communities upon graduation, providing high-quality, culturally sensitive care where it is needed most.
Growing Impact
The nation’s shortage of healthcare providers is a particular concern as the population ages.
“As the population grows and ages, there’s a dire need for healthcare,” Hill says. “Preparing PAs not only addresses the care shortage, but it also targets growing healthcare costs, as it costs less to educate PAs than medical doctors.”
Almost immediately after graduating, Chapman PAs make a difference in care settings.
“We receive great feedback about the preparedness of our students and graduates,” says Stephanie Saldivar, assistant professor and director of clinical education at Crean College. “Medical groups are approaching us to have students placed in their clinics.”
With the southernmost fully-accredited PA program in California, Chapman is poised to have an outsized impact on primary care in the region. Upon graduation, 33% of Chapman PAs choose to work in primary care, compared with the national average of less than 25%.
Making Specialists Accessible
While the need for primary care is great, specialty fields also are experiencing a shortage of physicians. In many specialties, PAs are able to assist with surgeries, which can reduce costs and streamline the delivery of care.
“If you call to get care from a specialist who doesn’t have a PA on staff, you could be on a waitlist for a few months,” says Anne Walsh, associate professor at Crean College. “But if a specialist has a PA, you may get in within a week or two.”
Katie Cornella (MMS ‘18) discovered her passion for a specialty – cardiology – during a rotation in Chapman’s PA Program. Now she works as a PA at the Orange County Heart Institute and Research Center.
It’s important work. Heart disease is the leading cause of death for both men and women.
Cornella experiences many rewards, including the chance to spend more time with her patients than is typically possible for physicians.
“That ultimately increases their confidence in the treatment plan,” Cornella says.

Popularity of the Program
Increasingly, students are drawn to the PA route for a host of reasons. PAs typically need just two additional years of school and training. The degree they earn, a master’s in medical science – PA studies, prepares them for state exams and then the workforce. Medical school takes four years to complete, in addition to at least two years of residency.
“I chose PA as my career because the schooling is expedited and I wouldn’t be so deep into student loans,” Cornella says.
PAs graduate into a job market that values their work. On average, they earn about $117,000 a year, but they can earn as much as $150,000. The bonus is that they typically work regular hours, which is a draw for many young adults.
Chapman PA graduate Casey Kupcha (MMS ’18) was attracted to the work-life balance. “If you enjoy treating people and being involved in clinical decision making, the PA route is a great option. It gives you more time to spend with patients and your family.”
Teaming Up for Better Care
Unlike the competition model at some medical schools, Chapman’s PA program encourages students to work together. After graduation, this collaborative approach can lead to better patient care.
“I consult with my Chapman classmates all the time,” Kupcha says. “If I have a strange EKG, I’ll take a picture and send it to them.”
The teamwork mindset “comes with the nature of being a PA,” says Saldivar, who also directs clinical education for Chapman’s PA program.
Saldivar, who works as a PA in a hospital emergency room, speaks to the culture of Chapman’s program: “We’re not just training people to get a degree; they’re going to be our colleagues,” she says.
Additionally, in many states, PAs benefit from legislation granting them a new measure of autonomy.
“Loosening supervision will help grow the number of primary-care PA practices in rural and underserved areas, where they are needed most,” Dean Hill says.
Moreover, PAs in California will be able to bill for their services, as physicians do, which will allow their work and impact to be tracked.
“More access to PAs means more access to care in general,” Saldivar says. “This is a really interesting time for PAs in California.”
Cornella agrees.
“It’s been my dream to be a part of medicine and give back to the community around me,” she says. “It’s an incredible experience.”



