Two PAs Use Genetics and Precision Medicine to Provide Answers and Develop Plans for Patients
All of Us Research Program Has Similar Goals
December 16, 2021
By Jennifer Walker
At the Greenwood Genetic Center (GGC) in South Carolina, PA Wesley Patterson finds great reward in helping patients who have unexplained symptoms and providing treatment plans so they can live full lives.
For example, Patterson might work with a child who has been diagnosed with failure to thrive after missing some developmental milestones. The child has likely been to multiple specialists and received uninformative test results. If Patterson suspects the child’s symptoms might be genetic, he can order appropriate genetic testing to identify a diagnosis and then tailor a treatment plan specifically for the child. This could include medication recommendations, additional blood work and imaging, and referrals to other specialists.

“In genetics, we consider ourselves the puzzle masters,” says Patterson, who is currently exploring genetics and genomics education for PAs as part of his Ph.D. program in healthcare genetics at Clemson University. “We take each piece of the puzzle—every symptom, every exam finding—and then we see if we can make those puzzle pieces fit together into a genetic syndrome. We use precision medicine to make sure these patients maximize their potential and prolong their lives by having the appropriate therapies, surveillance, monitoring, and specialty care that they need.”
Precision medicine takes into account differences in people’s genes, environment, and lifestyle to make personalized treatment plans that are the best fit for them. The National Institutes of Health’s All of Us Research Program has a goal of collecting this information from a diverse group of one million or more participants to help researchers learn the risk factors for certain diseases and discover what treatment plans will work best for people from different backgrounds. AAPA and the PA Foundation have partnered with All of Us to raise awareness about the importance of participating in research.
To understand how PAs can play a role in genetics and precision medicine, Patterson and his colleague at GGC, PA Laura Buch, talk about the power these fields have to provide patients and families with hope, answers, and appropriate treatment. They also share what they see as the importance of the All of Us Research Program, as well as why PAs might want to consider a career in the growing field of genetics.
Genetics helps patients find long-sought answers
Patterson, who is a founding member as well as treasurer and webmaster for the Society of PAs in Genetics and Genomics, entered the field of genetics almost by chance. When he was an undergraduate student studying animal and veterinary sciences at Clemson University, he walked by a poster that advertised an internship with the Greenwood Genetic Center. This nonprofit institute offers clinical services throughout South Carolina; comprehensive biochemical, cytogenetics, and molecular diagnostic testing; clinical trials and translational research; and educational outreach programs. Patterson applied and interned there during the summer between his junior and senior year.
A year later, when he was working at Kmart and figuring out his next career move, Patterson ran into an old GGC colleague, which led to a position as a laboratory technologist in GGC’s Molecular Diagnostic Lab for two years. Patterson left this position to attend the PA program at Radford University Carilion, formerly the Jefferson College of Health Sciences. In 2018, after graduation and working in family medicine for two and a half years, he found his way back to GGC when he received a call from the institute.
“They were interested in hiring their first PA,” Patterson says. “I jumped at the chance to get back to the GGC and practice in genetics.”
Today, Patterson evaluates and treats a wide range of patients who are referred to GGC for genetic evaluation. These patients can have a variety of symptoms and challenges, including intellectual disability, autism spectrum disorder, developmental delay, hearing loss, and seizures, and in many cases the patients or their families have been searching for the cause of these symptoms for some time. Genetic testing can finally lead to a diagnosis and subsequent treatment plans.
“When you’re able to give a family an answer after they’ve been on this long diagnostic odyssey, explaining that this is why [their symptoms] happened and these are some things we can do to help, that’s the best feeling in the world,” Patterson says.

Genetics saves lives and gives patients day-to-day freedom
Like Patterson, PA Laura Buch didn’t plan to enter the field of genetics. After working as a medical scribe for a family practice, she completed the PA program at Elon University and moved to South Carolina to be with her now-husband. Buch thought she would work in family practice again because she wanted to establish long relationships with patients and continue to care for them throughout their lifetime. But when she was sent a job posting for a Metabolic Advanced Practice Provider Fellowship at GGC—a posting that Patterson created—she was drawn to the role, which she thought would offer the same opportunity to provide continuous and compassionate care. Buch applied and completed the fellowship earlier this year.
Now Buch specializes in treating patients who have been diagnosed with metabolic conditions, particularly lysosomal storage disorders. These are metabolic diseases that lead to enzyme deficiencies and ultimately cause toxic build-up of waste products in the body’s cells, resulting in a variety of symptoms, according to the National Organization for Rare Disorders.
In her biomedical metabolic clinic, Buch also sees patients who have had abnormal newborn screens. If a genetic diagnosis is confirmed, individualized treatment plans for infants can include dietary changes, supplements and medications, and opportunities to participate in clinical trials.
To illustrate the power of genetics, Buch talks about a baby whose newborn screen and subsequent genetic testing confirmed a diagnosis of Pompe disease. This severe and progressive lysosomal storage disorder can cause low muscle tone, muscle weakness, cardiac enlargement, respiratory difficulties, and eventually death in infants.
“Luckily for this family and for other families to come, the state of South Carolina began screening for Pompe disease in February 2021,” Buch says. “We knew how important it was to the family that we were able to detect this condition so early on and start their child on treatment as soon as we did [because] with Pompe disease every hour counts. [With a quick diagnosis], we can get patients on treatment with weekly infusions [ideally] before two weeks of age and ultimately save their lives.”
Genetics can also open up more convenient treatment options for patients through precision medicine. Gaucher disease is a lysosomal storage disorder which leads to a build-up of fatty substances in organs like the spleen and liver due to enzyme deficiency. The affected organs can become enlarged, and their function is adversely affected as a result. Usually patients require bi-weekly visits to an infusion center to receive enzyme replacement therapy for several hours. But Buch is able to order genetic testing for a variant in the CYP2D6 gene to see if a patient who has been diagnosed with Gaucher disease may respond to Eliglustat, an oral medication, instead of receiving the bi-weekly infusions.
“This option in treatment modalities gives them a lot more freedom in their daily lives,” explains Buch, who takes great pride in being able to help patients navigate the complicated world of rare diseases. “The implications of being able to get the correct treatment for a patient who is eligible for it and amenable to it are significant. We can see improvements in quality of life, access to care, and overall longevity. Genetic testing changes the lives of patients every day.”

All of Us Research program helps build a diverse health database
The All of Us Research Program is working to accelerate this shift toward precision medicine by collecting genetic, environmental, and lifestyle data from participants from different backgrounds who reflect the diversity of the United States. The program aims to build one of the most diverse health databases available—a goal that Patterson appreciates.
“A lot of our research in genetics is based on the Caucasian population over the last 40 years,” he says. “[But the All of Us Research Program] is not just based on one group. It’s going to be truly representative of individuals in the United States and the world, which is important because some changes [in genes] are more commonly found in certain populations. Even medication management is a little different depending on the genotype of our patients. So having that information [from the database] could help from a [patient care] aspect.”
In addition to helping diversify the research base, participants can also learn about themselves. The program has been returning genetic results to participants who provided samples so they can learn what their DNA says about their health. The program also provides access to genetic counselors to help answer questions from participants and their healthcare providers.
Although some patients may not feel comfortable submitting their genetic information, Patterson and Buch think PAs have an opportunity to encourage involvement in All of Us by telling their patients about the program. With a strong provider-patient relationship, a patient might feel more comfortable asking their PA questions about the program, and the PA can address some of the patient’s concerns.
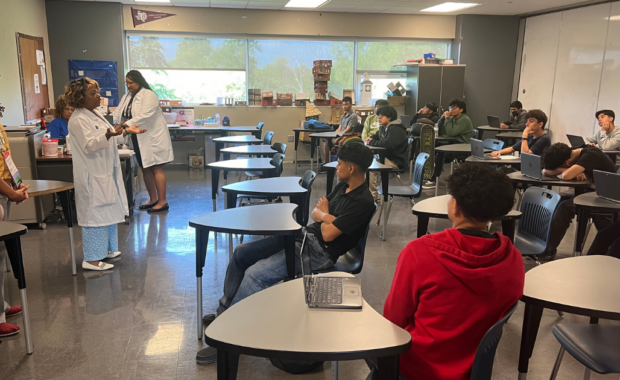
PAs may also want to consider practicing in genetics. Patterson and Buch jointly lead workshops on genetics at PA programs across the East Coast, where they share their passion, expertise, and experiences to educate practicing PAs and PA students about this exciting field.
“With all the advances in medicine, especially in genetics and technology, there’s more of a need for genetic healthcare providers,” says Patterson, adding that there are about 20 PAs working in genetics across the U.S. currently – and he only sees that number increasing. “PAs can come into the field of genetics and help fill that workforce gap, so we want to encourage them to consider this very rewarding specialty.”
Jennifer Walker is a freelance writer in Baltimore, MD. Contact Jennifer at [email protected].
You Might Also Like
Colorado PAs Spotlight All of Us Research Program
PAs: Get Involved in Genetics to Help Patient
PAs Say Genetics and Genomics Key to Patient Diagnosis and Treatmen
PAs Can Apply for the NIH/ACMG Genomic Medicine Program Management Fellowship