Charting CME on Health Disparities Leads to Positive Changes in PA Practice
Outside the Box Successful in Educating on Health Disparities
January 21, 2020
By AAPA Research Department
Outside the Box: Reducing Health Disparities CME was designed to educate PAs on health disparities, with the aim of improving practices among participants in five domains including:
- Race and ethnicity
- Sexual orientation and gender identity (SOGI)
- Literacy (including numeracy)
- Physical, sensory, or cognitive disabilities
- Economic and geographic factors
Designed and analyzed by PAs and PA researchers
The team that designed Outside the Box included Kim Zuber, PA-C, MS, executive director of the American Academy of Nephrology PAs; Diane Bruessow, MPAS, PA-C, secretary-treasurer of AAPA, instructor of the PA Online program at Yale University, and clinician in New York and New Jersey; Patricia J. Devine, MLS, community outreach coordinator of the HEALWA program at the University of Washington; and Howard O. Straker, EdD, PA, MPH, president of the Physician Assistant Education Association and an assistant professor and director of the PA/MPH program at The George Washington University. Timothy C. McCall, PhD, associate director of surveys and analysis at AAPA, also joined the team to assist with research methodology, statistical analysis, and interpretation of the results. The idea for Outside the Box followed CME called Kidneys in a Box, inspired by Zuber.
Analysis of Outside the Box CME completed by PAs between 2017 and 2019 has shown that an innovative approach involving charting and treatment can change PA behavior.
The Outside the Box program, which launched in 2015, asked PA participants to review 10 random charts from their practice and answer a battery of questions about each chart, documenting how they identified and/or altered treatment plans based on this information. Examples of the questions asked were “Did you ask the patient about their sexual behaviors?” (yes or no) and “How did this affect the health screening that you conducted?” Response options were: “Conduct the same screenings as usual,” or “Conduct one or more screenings specifically based on the patient’s behavior.” After this chart review, participants were given a percentage score for each domain – that is, the percentage ideal charting behaviors across the charts (i.e., each social determinant of health is ideally recorded in the chart, and this information is considered when deciding on a plan of care).
Implementing practice-specific interventions
Following the pre-intervention chart review, participants were given educational materials related to health disparities in each of the domains of interest (sexual orientation and gender identity [“SOGI”], race and/or ethnicity, health literacy and/or numeracy, physical, cognitive, and/or sensory disabilities, and economic or logistic insecurity). Participants implemented practice-specific interventions based on the educational materials.
Participants in the analysis included 102 clinically practicing PAs studied over a two-year period. The average experience in clinical practice for the cohort was 8.9 years and PAs saw 68 patients per week on average. Specialties represented among the cohort were primary care (31.1%) followed by surgical specialties (29.1%), internal medicine subspecialties (13.6%), emergency medicine (6.9%), and others (15.3%). Four percent identified no medical specialty, and most participants were from the South and the West.
Analysis of results
Study results are summarized in the January 2020 issue of JAAPA in an article titled Improving health disparities in PA practices: A quality improvement study.
Thirty days after the initial chart review, participants again selected ten different charts at random (a post-intervention chart review) and answered the same battery of questions. Afterwards, participants were given their pre-intervention ideal behaviors percentage scores, as well as their post-intervention ideal behavior percentage scores to see how their behavior compared to initial responses.
After participants completed the Outside the Box CME, the researchers calculated whether significant changes in ideal charting behavior resulted one month after the educational intervention. Results indicated that after completing Outside the Box, PAs showed significant improvements across each of the five domains. Not only were the results statistically significant, but the magnitude of the differences was moderate to large in all cases except economic and logistics.
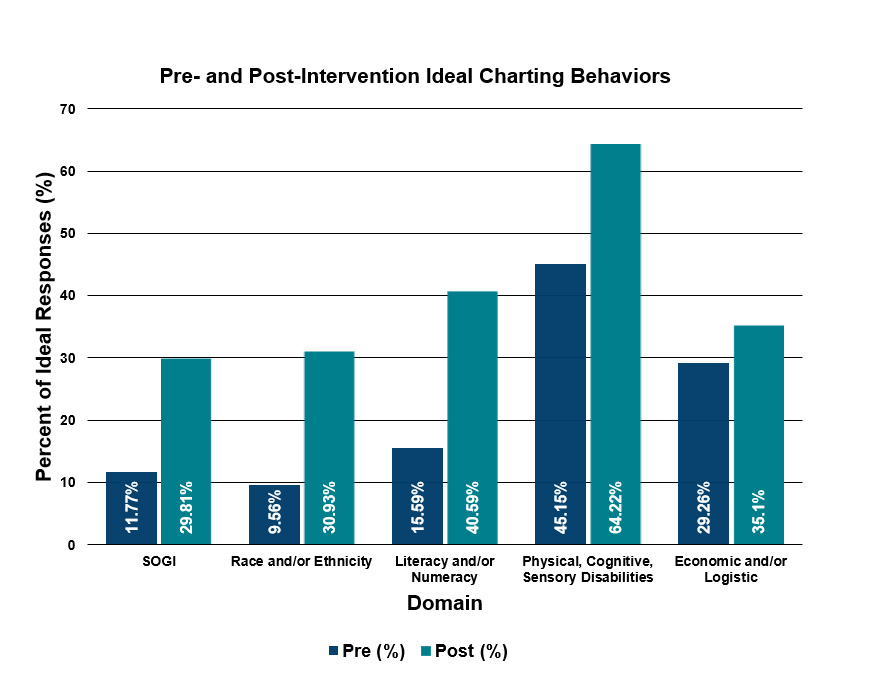
Participation in the Outside the Box program led to practice quality improvements related to domains known to influence health disparities. While the researchers were disappointed that even the post-intervention behaviors failed to reach >50% in four of the five domains, the improvements were significant and promising. Results are suggestive that increasing awareness of ideal professional behaviors can result in quality improvements in PA practices. This program is a first step in addressing health disparities by provider behavior change through education. The authors hope to assess next the stability of these improvements over time.
Author is Tim McCall, PhD, associate director, surveys & analysis at AAPA. Contact Tim at [email protected]. Co-authors of the research described in this article are Zuber, Bruessow, Devine, and Straker.
Read More:
Improving health disparities in PA practices: A quality improvement study (JAAPA, January 2020)
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



