PAs Tout Benefits of Vaccines Despite Persistent ‘Anti-Vaxxers’
Building Trust with Patients Best Approach
August 20, 2019
By Dave Andrews
Vaccines continually save millions of lives each year by helping control and prevent dozens of potentially deadly diseases. Still, the voices of numerous anti-vaccination groups only seem to grow louder.
Many providers attribute the “anti-vax” movement to widespread misconceptions and inaccurate information about the side effects of various vaccines. National Immunization Awareness Month in August gives providers even more reason to look for opportunities to clarify any misunderstandings and foster an open dialogue with their patients about immunizations.
Michelle Kerr, PA-C, has witnessed firsthand the evolution of the anti-vaccine movement, having worked predominantly in pediatrics since the mid-90s. In addition to her clinical practice, Kerr serves a dual role as the assistant specialty medical director for three children’s urgent care centers and is the chief advanced practice provider (APP) for the urgent care division of Atrium Health in Charlotte, North Carolina.
“When I first started, it seemed nearly everyone was on board with vaccines. People didn’t even question it back then,” Kerr said. “The mindset was largely, ‘Great, I no longer have to worry about my child getting measles, chickenpox and tetanus and so many other illnesses that used to be very common and even fatal, but that have largely diminished thanks to vaccines.’”
[Measles Cases in U.S. Are Highest Since Measles Was Eliminated in 2000]
As chief APP, Kerr oversees 30 urgent care locations and more than 120 advanced practice providers, so she is acutely aware of the opposition providers increasingly face regarding immunizations. In her opinion, the shifting perceptions largely correlate with a growing awareness of certain health disorders— primarily autism—and for many, a need to hold something or someone accountable.
“It’s just human nature to grasp at possible causes in an effort to answer the why,” Kerr said. “That element of fear often makes people reach out for any kind of answer, even if it isn’t based on medical evidence. People choose to believe what they want to believe and unfortunately, a large number of people choose to blame vaccines.”

Movement Toward All- Natural Healing
Similar apprehensions regarding vaccines have become increasingly common in rural areas as well. For more than 11 years, Sarah McQueen, PA-C, has worked at Dayspring Health in Williamsburg, Kentucky, serving as the center’s vaccine coordinator. Within her patient population, vaccine refusals frequently stem from either cultural differences or religious beliefs, but McQueen says there is also a growing distrust of modern medicine and a movement toward all-natural healing.
“I think most people have good intentions with this all-natural movement,” McQueen said, “but it can become problematic for those who believe everything natural is good for you, which we know isn’t true. There are lots of natural things that can be harmful, just as there are many things that are not natural that can be completely safe and even necessary.”
McQueen says there are also many patients on the fence about immunizations and choose to only vaccinate for the diseases they think are the most severe, while disregarding others they consider to be extraneous.
“It’s interesting that the HPV vaccine is often the one that gets the most opposition, especially in very conservative areas like where we are,” McQueen said. “People equate HPV solely with sexual activity and think, ‘Well, my kids are not going to be sexually active, therefore, they don’t need that.’ But they’re overlooking the fact that the vaccine also helps prevent many types of cancer.”
[Society of PAs in Family Medicine]
Less Willingness to Listen
Seeing patients who continually refuse flu and HPV vaccines is nothing new to Kate Shand, PA-C, even though her clinic, Legacy Pediatrics in Rochester, New York, is very open about its pro-vaccine stance.

“The biggest change I’ve seen over the years is an unwillingness among many patients to even listen to their providers on the topic of immunizations,” Shand said. “Some just want to shut us down and not talk about it.”
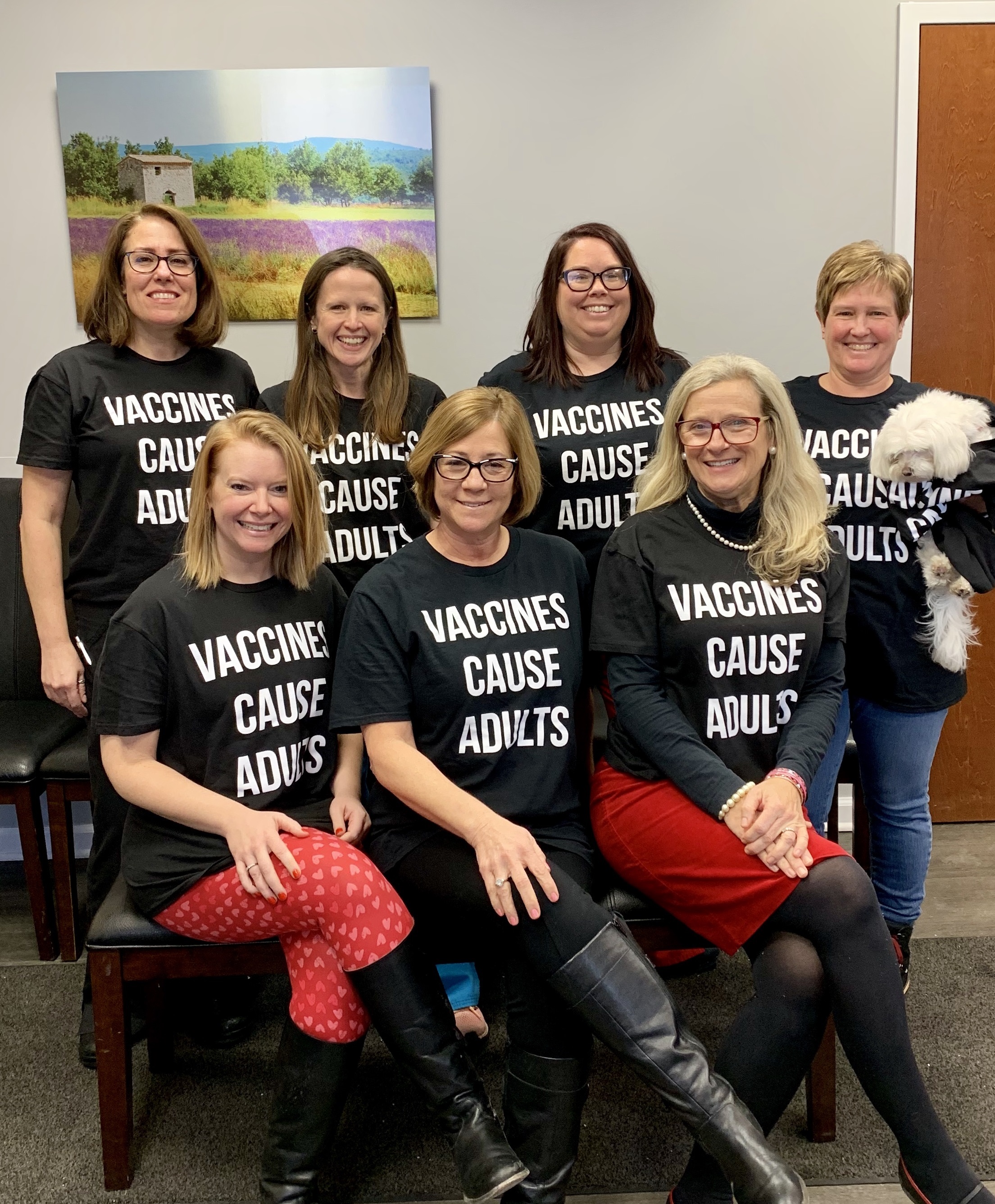
Shand and some of her colleagues made a social media stir recently when they posted a picture of themselves to the clinic’s Facebook page. They were wearing custom T-shirts that read “Vaccines Cause Adults,” a play on the phrase “vaccines cause autism” which is commonly used by anti-vaccination groups.
The photo quickly went viral and was even highlighted by several local news outlets. Shand said the clinic immediately received countless positive comments and calls of support from other providers and groups across the country.
But as expected, they were also bombarded with a large number of negative comments from anti-vaccination groups. Shand said it was tough to look past some of the negativity, but it quickly died down after about a week.
[Vaccine Safety Letter to President Trump]
“The whole reason we put ourselves out there like that was because we’re tired of seeing the anti-vax movement having such a loud voice [while] everybody else just stays quiet,” Shand said. “Eventually, you just have to say enough is enough. We believe in this. This is our stance and we aren’t afraid to put it out there. I think that needs to happen more.”
Shand said they received so many requests to purchase the shirts, they decided to make more and sell them to raise money for charity. So far, they’ve raised more than $4,000, all of which has been donated to a local children’s hospital and the PolioPlus program run by the Rotary Club of Rochester.
The Right Approach
McQueen acknowledges it can be difficult to know how to approach someone who opposes vaccinations. And the last thing a provider would want to do is come across as combative.
“It’s easy to get snarky or cynical about how ‘Dr. Google’ might seem to know more than the actual provider,” McQueen said. “Doing so might make you feel better initially, but that doesn’t help the situation.”
The main objective, she says, is to establish trust. “Taking the time to get to know each patient on a personal level is key so you can ask them what their reservations are about vaccines and what factors drove their decision making,” McQueen said. “Knowing those answers will help you determine how—or if—the patient’s concerns can be addressed productively in the clinic.”
Shand agrees that successful outcomes depend on building trust. She suggests leaving questions open-ended to find out why the patient feels a certain way and what are their specific fears.
“This is a very personal decision that, ultimately, is up to the patient,” Shand said. “But little by little, we as providers need to effectively educate the patient as best we can to help them make the decision that’s right for them.”
More Resources
National Immunization Awareness Month CDC Digital Communication Toolkit
Dave Andrews is a freelance writer and public relations professional based in Northern Virginia. Contact him at [email protected].
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



