Diabetes is Daunting. Finding a Quality Provider Shouldn’t Be.
PAs Provide Quality Diabetes Care Management
November 13, 2018
By AAPA Research Department

Across the United States, 30.3 million adults live with diabetes1 and another 84.1 million live with prediabetes.2 Shockingly, 90% are unaware that they have prediabetes, which untreated often leads to diabetes within five years.2 Those who lack access to health services have increased odds of being unaware; however those with insurance but no regular healthcare provider have the highest odds of being unaware of being prediabetic.3 PAs can greatly expand access and care via telehealth, which can ultimately help prevent type 2 diabetes. The success of telehealth in preventing type 2 diabetes in high-risk adults has been demonstrated by the NIH’s Diabetes Prevention Program (DPP).4
It is clear that PAs play an important role in the management and prevention of diabetes. In fact, AAPA research shows that 86.8% of PAs see patients with type 2 diabetes. Even with a complex diagnosis such as diabetes, patients can depend on the quality of the care provided by PAs. Research has demonstrated that the quality of care provide by PAs to diabetic patients has been shown to be comparable to the care provided by a physician.5
PAs provide comparable diabetes care to physicians and NPs.
In a clinical research study that analyzed the management of patients with diabetes from diagnosis through a four-year follow-up period, researchers found that care delivered by PAs was comparable to that of physicians and NPs.5 This supports previous research findings that the inclusion of PAs benefits team-based care and management of diabetes.6,7 A large concern in diabetes management is improving treatment adherence. Not only does better adherence improve outcomes, but it is also cost effective.8 Preliminary research highlights that improving patient-provider communication can also positively influence treatment adherence.9
PAs are caring for patients with diabetes on a weekly basis.
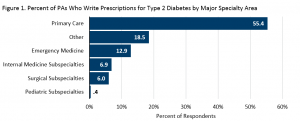
In 2017, AAPA surveyed PAs on their prescribing patterns. In a typical week, 44.5% wrote at least one prescription for Type 2 Diabetes. Across all major specialty areas, PAs in primary care most frequently reported writing at least one prescription in a typical week (Figure 1).
Nearly 3 in 5 PAs write up to 25% of prescriptions for type 2 diabetes.
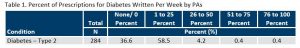
As the seventh leading cause of death11, the effective management of diabetes at the early stages contributes to better health outcomes for the patients. Not only do people with diabetes deal with issues in regulating blood sugar, but also diabetes is often comorbid with other serious conditions including hypertension, hyperlipidemia, and/or obesity. In fact, only 14% of people with type 2 diabetes did not have a comorbidity.12 Although AAPA research shows that three out of five PAs indicated anywhere from one to 25 percent of all their prescriptions written each week were for type 2 diabetes, the total number of prescriptions written related to diabetes is likely much higher when those for written for common comorbidities of diabetes (i.e., hypertension, high cholesterol, obesity) are taken into account.
What does the future in diabetes management hold for PAs?
Barriers such as not having full prescriptive authority or scope of practice determined at the practice level may prevent PAs from delivering diabetes care now and in the future.13 Expanding the roles of PAs could mean opening more access to quality care management for diabetes. PAs who are highly educated and trained in team-based care will continue to be leaders of diabetes care teams, and as such, need to be prepared for this role. Courses such as AAPA’s free Diabetes Leadership Edge CME Track give PAs the tools to effectively manage and treat this growing health concern.
More Resources
Diabetes Leadership Edge CME Track
National Health Quality Initiatives
References
- Centers for Disease Control and Prevention. Type 2 Diabetes. August 15, 2018; https://www.cdc.gov/diabetes/basics/diabetes.html. Accessed October 31, 2018.
- Centers for Disease Control and Prevention. Prediabetes: Your Chance to Prevent Type 2 Diabetes. June 25, 2018; https://www.cdc.gov/diabetes/basics/prediabetes.html. Accessed October 31, 2018.
- Campbell TJ, Alberga A, Rosella LC. The impact of access to health services on prediabetes awareness: A population-based study. Prev Med. 2016;93:7-13.
- Vadheim LM, Patch K, Brokaw SM, et al. Telehealth delivery of the diabetes prevention program to rural communities. Transl Behav Med. 2017;7(2):286-291.
- Yang Y, Long Q, Jackson SL, et al. Nurse Practitioners, Physician Assistants, and Physicians Are Comparable in Managing the First Five Years of Diabetes. Am J Med. 2018;131(3).
- Everett C, Thorpe C, Palta M, Carayon P, Bartels C, Smith MA. Physician Assistants And Nurse Practitioners Perform Effective Roles On Teams Caring For Medicare Patients With Diabetes. Health Aff. 2013;32(11):1942-1948.
- Federman DG, Krishnamurthy R, Kancir S, Goulet J, Justice A. Relationship Between Provider Type and the Attainment of Treatment Goals in Primary Care. Am J Manag Care. 2005;11(9):561-566.
- Kennedy-Martin T, Boye K, Peng X. Cost of medication adherence and persistence in type 2 diabetes mellitus: a literature review. Patient Prefer Adherence. 2017;11:1103-1117.
- Freeman-Hildreth Y, Aron D, Cola P, Want Y. Provider Attributes that Influence Diabetes Adherence. Poster presented at: Physician Assistant Education Association Education Forum; October 26, 2018; Anaheim, California.
- Hooker RS, Cawley JF, Leinweber W. Career Flexibility Of Physician Assistants And The Potential For More Primary Care. Health Aff. 2010;29(5):880-886.
- Centers for Disease Control and Prevention. About Diabetes. June 1, 2017; https://www.cdc.gov/diabetes/basics/diabetes.html. Accessed October 31, 2018.
- Suh D-C, Choi I-S, Plauschinat C, Kwon J, Baron M. Impact of comorbid conditions and race/ethnicity on glycemic control among the US population with type 2 diabetes, 1988–1994 to 1999–2004. J Diabetes Complications. 2010;24(6):382-391.
- Valentine V. Your Diabetes Care Provider in the Future Is Probably an NP or PA! Clin Diabetes. 2014;32(4):145-147.
Image Source
Apples Diabetes Elta The Meter Satellite Express. 2016. Available at: https://www.maxpixel.net/Apples-Diabetes-Elta-The-Meter-Satellite-Express-3612851. Accessed November 13, 2018.
About the data
Data on diabetes management are derived from the 2018 August and November AAPA National PA Practice Survey.
Author is Elaine Slaven, BS, a research associate at AAPA. Contact us at [email protected].
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



