Hospital ER PA and MD Make Three Changes to Improve Teamwork
PA and MD to Speak at ELC about the Power of Collaboration
September 21, 2018
By Jennifer Walker
Collaboration may be the key to being an effective leader. “Regardless of how creative, smart and savvy a leader may be, he or she can’t transform an organization, a department or a team without the brain power and commitment of others,” writes Carol Kinsey Goman, PhD, a body language coach, in Forbes.

At AAPA’s Center for Healthcare Leadership and Management’s Executive Leadership Conference (ELC), the “Team Management Skills” panel will focus on why collaboration is important in healthcare and how leaders can work together to improve patient care. Puja Mody, PA-C, and Marrissa Baker, MD, of Vituity, a healthcare staffing company, will lead the session.
“We’ll really be stressing including the whole team when you are trying to implement a process change, building a good rapport between all providers, and using soft skills that are needed to work together as a team,” Baker says.
Through Vituity, Mody and Baker work in the emergency department at St. Agnes Hospital in Baltimore, Maryland. Here, Mody, the lead PA for the ER, and Baker, the advanced provider liaison—advanced providers at Vituity include PAs, NPs, and certified registered nurse anesthetists (CRNAs)—have collaborated with each other and other members of the department to streamline operations and make adjustments to benefit patients and staff.
Here are three changes that staff in the St. Agnes ER have made as a result of their willingness to collaborate across providers:
They streamlined operations to better serve patients.
The St. Agnes ER has bi-weekly operations meetings which are attended by representatives from all of its departments, including provider leadership, nursing, phlebotomy, diagnostic imaging, registration, and security. Through these meetings, St. Agnes has implemented processes to better serve patients. For example, the team decided to change the ER’s front-end process. “Now a PA screens every patient who comes through the door,” says Mody, who has attended these collaborative meetings since 2014. “This makes sure that the appropriate workups are put in initially to help expedite patient care and recognize potentially critical patients.”

They ensured that advanced providers have support.
The 11 full-time PAs in St. Agnes’ ER primarily staff the Rapid Medical Evaluation Area (RME), an area for low-acuity patients, while physicians primarily staff the main ER. Recently though, the physicians and the advanced providers decided to move a physician from the main ER to the RME, and one PA from the RME to the main ER. “This creates a collaborative approach to patient care in all areas of the ED, [and] advanced providers have physician support while working with high-acuity and low-acuity patients,” Mody says.
They started an internship program for advanced providers.
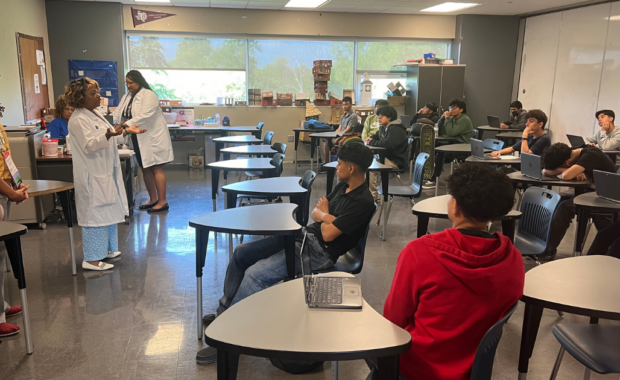
This past January, Mody and Baker worked together to create an internship program for PAs who are new graduates and who are interested in working in the ER. They had the idea for the internship after realizing that the new PAs they hired were overwhelmed. “As a new grad, it can be hard to come into the emergency department and start working independently,” Mody says. “We wanted to give new PAs a robust program where we could give them support and gradually transition them to the ER.” Vituity has its own internship program for advanced providers, which the company has rolled out at several sites in the Midwest; Mody and Baker used this as a framework for their program but made adjustments as needed to fit their site.
During the 12-week internship program, which is offered on a rolling basis, advanced providers spend six weeks with a physician in the main emergency department and six weeks in the Rapid Medical Evaluation Area. Physicians and other PAs might also offer lectures that advanced provider interns can take part in. Six lectures were offered in the last internship cycle, covering topics such as orthopedics, neurology, EKGs, abdominal pain, the cardiovascular system, and the genitourinary system. So far, three PAs have completed the internship program, and they all work in the ER at St. Agnes.
“Our internship program is really about investing in new grads or any provider who is new to emergency medicine and giving them the skills that are specific to working in the emergency department,” Baker says.
Why Should PAs attend the ELC?
When asked about how ELC can benefit PAs, Baker says, “Just hearing other people’s experiences and seeing what others have done to get the ball rolling at their sites can be beneficial.”
Mody—who, as the lead PA, is the liaison between the 11 other PAs and the management at St. Agnes—also points out that leadership isn’t a subject that was taught in PA school. “We studied medicine, so we know medicine. But I think it’s hard to be an effective leader because that’s not what we studied,” Mody says. “This conference gives us an educational opportunity to be more efficient and effective leaders.”
CHLM’s Executive Leadership Conference will tak place on Nov. 6-8, 2018.
Jennifer Walker is a freelance writer in Baltimore, MD. Contact Jennifer at [email protected].
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.