PAs Can Bring Cost-Effective Care to Complex Patients
An Opportunity for Care Coordination
April 12, 2018
By AAPA Research Department
Adults aged 65 and older frequently have multiple chronic conditions that may add to their medical complexity. Treatment for complex patients is unsustainably costly, but the needs of these patients can be met with effective care strategies. PAs are poised to take lead roles in bringing cost-effective care coordination to complex patients.
Super-Utilizers: Not So Super
Superheroes may save the day, but “super-utilizers” can break the bank. Super-utilizers are aptly named to reflect the small segment of the population that utilizes healthcare the most. In fact, just 5% of the population accounts for over half of all healthcare spending 1. These super-utilizers are often patients with multiple, complicated conditions in combination with additional factors that may make them medically complex. The costs for treating patients with multiple chronic conditions has been estimated to be up to seven times as much as treating patients with only one chronic condition1. Research has shown, however, that healthcare costs can be reduced through effective care-coordination strategies 2,3,4. By providing effective care-coordination and assuming care-coordinator roles, PAs can enhance their marketability as a cost-effective resource.
The Cost of Care
According to the Centers for Disease Control and Prevention (CDC), nearly half of all adults have at least one chronic condition, and one out of four adults have two or more chronic conditions5. In adults 65 and older, this number grows to three out of four people who have multiple chronic conditions (MCC)5. With each additional chronic condition, there is a large increase in per capita Medicare spending. To put this into perspective: 2015 per capita spending for those with zero to one chronic conditions was $1,867; spending for those with six or more conditions was $32,136 6.
Increased frequency of health visits and hospital readmissions are, in part, driving the high cost of MCC. Of those with zero to one chronic conditions, only 4% had 13 or more doctor visits per year. In contrast, 46% of those with six or more chronic conditions visited their doctor 13 or more times. Hospital readmissions are similarly dominated by patients with multiple conditions. In fact, 98% of hospital readmissions in 2010 were patients with two or more chronic conditions. Furthermore, the majority of all clinician visits (64%), all prescriptions (83.1%), all home healthcare visits (87.5%), and all inpatient stays (70.4%) are all resulting from patients with MCC 7.
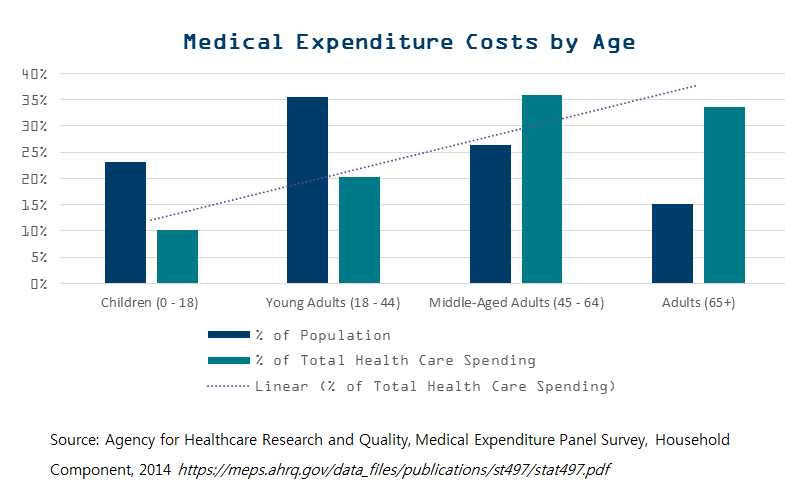
It is easy to see how MCC, which can add to the complexity of patient care, can also add dollars. Because MCC are more prevalent in adults 65 years and older 6, it is unsurprising that this age group is also one of the costliest. When we look across age categories, we see that adults aged 65 and older make up the smallest percent of the total population (15.1%) yet account for 33.6% of the total health care spending8.
Time to Coordinate
Care for medically complex patients is a high priority – not only because these patients are highly prevalent, but because managing costs benefits patients, healthcare providers, and health systems. Medically complex patients are high-need patients that frequently require coordination between multiple medical providers. Lack of coordination can result in complications, declines in functional status, increased dependency, and other negative health outcomes for patients and major costs for healthcare providers 9. The cost of waste associated with poor care coordination has been estimated to be between $25 and $45 billion 9. Others have found that patients with poorly coordinated care had a 75% higher cost compared to those with coordinated care 10.
The current cost of healthcare spending is unsustainable. With effective care strategies, this cost can greatly be reduced. A successful care coordination program at Gunderson Health, for example, targeted medically complex patients and emphasized team-based care 4. With the use of care coordinators, after 24 months the program saw a 64% reduction in unplanned charges, 60% reduction in total charges, and 46% reduction in length of hospital stays for care coordination patients 4. As the need to reduce healthcare costs increases, care coordinators and team-based models become critical.
What it Means for PAs
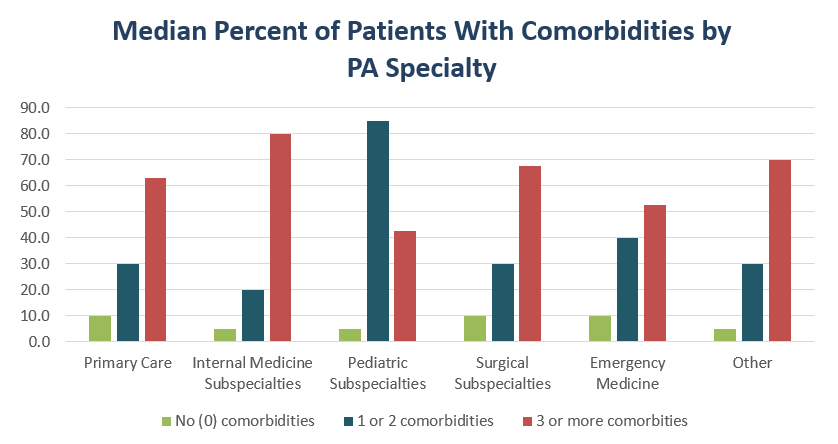
PAs of all specialties regularly see complex patients. Using a typology developed with physicians, complex patients include those with complex medical illnesses, socioeconomic challenges, mental illnesses, and/or difficult behaviors and traits11. In looking at the median percent of patients seen, PAs indicated that 50% of their patients have medical complexity, 50% have socioeconomic challenges, 25% have a mental illness, and 20% exhibit difficult behaviors or traits. Further, 91% of PAs indicated that they see patients 65 years and older, a demographic that frequently has multiple chronic conditions. Across all PA specialties, the majority of their patients have comorbidities except pediatrics; the largest percentage of their patients have 3 or more comorbidities (AAPA unpublished data, 2018).
Programs that have experienced care-coordination cost benefits call specifically for care coordinators, which may be any medical professional. Previous research illustrates that PAs are a cost-effective resource for providing medical care, care coordination, increasing patient access, and improved patient quality 12-15. PAs regularly see complex patients. They are poised to assume these care-coordinator roles and help to bring drastic reductions in healthcare costs.
More Resources
About MCC
About Care Coordination Model at Gunderson
Authors are Elaine Slaven, AAPA’s research associate, and Noël Smith, MA, AAPA’s senior director of research. Contact them at [email protected].
References
- Stanton M, Rutherford, MK. The High Concentration of U.S. Health Care Expenditures. Agency for Healthcare Research and Quality. 2005(Research in Action Issue 19).
- Mangiante L. Intensive Outpatient Care Program (IOCP) Coordinating Care for Those Who Need it Most. Pacific Business Group on Health. 2014.
- Stremikis K, Connors, C., Hoo, E. Intensive Outpatient Care Program: A Care Model for the Medically Complex Piloted by Employers. Commonwealth Fund. 2017.
- Berry L, Rock, B., Houskamp, B., Brueggeman, J, Tucker, L. Care Coordination for Patients With Complex Health Profiles in Inpatient and Outpatient Settings. Mayo Clinic Proceedings. 2013;88(2):184-194.
- Ward B, Schiller, J., Goodman, R. Multiple Chronic Conditions Among US Adults: A 2012 Update. Preventing Chronic Disease. 2014;11:1-4.
- Chronic Conditions Charts: 2015. CMS. 2015.
- Gerteis J. ID, Deitz D, LeRoy L, Ricciardi R, Miller T, Basu J. Multiple Chronic Conditions Chartbook. AHRQ Publications. 2014.
- Mitchell E. Concentration of Health Expenditures in the U.S. Civilian Noninstitutionalized Population, 2014. Agency for Healthcare Research and Quality. 2016; Statistical Brief #497.
- Berwick DMaH, A.D. Eliminating waste in US health care. JAMA. 2012;307(14):1513-1516.
- Owens MK. Costs of uncoordinated care. in: P.L. Yong, R.S. Saunders, L.A. Olsen (Eds.) 0The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. National Academy Press. 2010:109-114.
- Loeb D BI, Candrian C, E B. Primary Care Physician Insights Into a Typology of the Complex Patient in Primary Care. The Annals of Family Medicine. 2015;13(5):451-455.
- Goldberg DG BT, Kuzel AJ, Love LE, Carver MC. Team-based care: a critical element of primary care practice transformation. Population Health Management. 2013;16(3):150-156.
- Cawley JF HR. Physician assistants in American medicine: the half-century mark. The American Journal of Managed Care. 2013;19(10):333-341.
- Glotzbecker B, Yolin-Raley DS, DeAngelo DJ, Stone RM, Soiffer RJ, Alyea EP. Impact of Physician Assistants on the Outcomes of Patients With Acute Myelogenous Leukemia Receiving Chemotherapy in an Academic Medical Center. Journal of Oncology Practice. 2013.
- Roy CL LC, Lund M, Boyd C, Katz JT, McKean S, Schnipper JL. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. Journal of Hospital Medicine. 2008;3(5):361-368.
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



