Autism Spectrum Disorder in the Clinical Setting
PAs Should Look for ASD When Managing Pediatric Patients
April 2, 2018
By AAPA Research Department
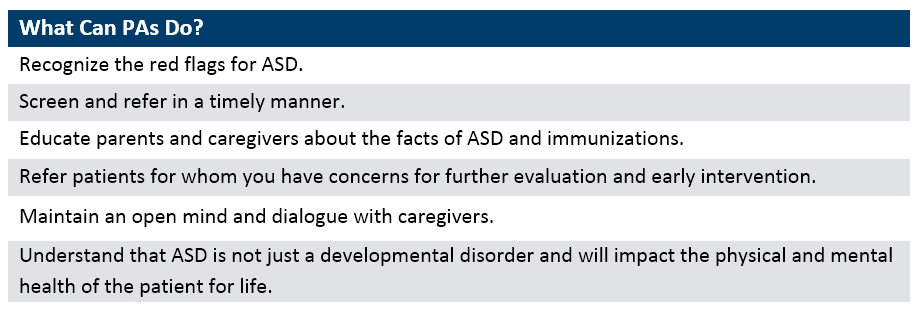
Medical providers such as PAs are often the first point of contact for caretakers of children with Autism Spectrum Disorder (ASD) and as such, need to be comfortable speaking about how to identify red flags of ASD, and where to refer caretakers if there is any concern.
What is Autism Spectrum Disorder?
Autism Spectrum Disorder is a broad term that captures a spectrum of previously separate diagnoses including Autistic Disorder, Asperger Disorder, and Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS). The broadness of ASD allows for developmental disorder to be classified by severity rather by separate diagnosis. Research points to a multitude of factors with a strong genetic basis.1,2 Characteristic to ASD are varying severities of social, communication, and behavioral problems. Although many children with ASD may learn differently, an intellectual disability is not present in all cases nor is it required by diagnostic criterium. Understanding the varying signs and symptoms of ASD is critical for early diagnosis and assessing the amount of daily care that may be needed.2,3
Prevalence
According to the Centers for Disease Control and Prevention (CDC) and the Autism and Developmental Disabilities Monitoring (ADDM) Network, about 1 in 68 children have been identified with autism spectrum disorder. White children compared to black or Hispanic children are at higher risk; however, the disorder is present in all racial, ethnic, and socioeconomic groups.2,3 Across gender, there is a much higher prevalence of ASD in males than females. In fact, ASD is about 4.5 times more common among boys (1 in 42) than among girls (1 in 189).2 It is interesting to note that almost half of children with ASD had average to above average intelligence. The ADDM network found intellectual disability was prevalent in only 31.6% of ASD cases, with 24.5% borderline, and 43.9% classified as average or above average. The presence of intellectual disability was more likely in women than men.4
Diagnosing ASD
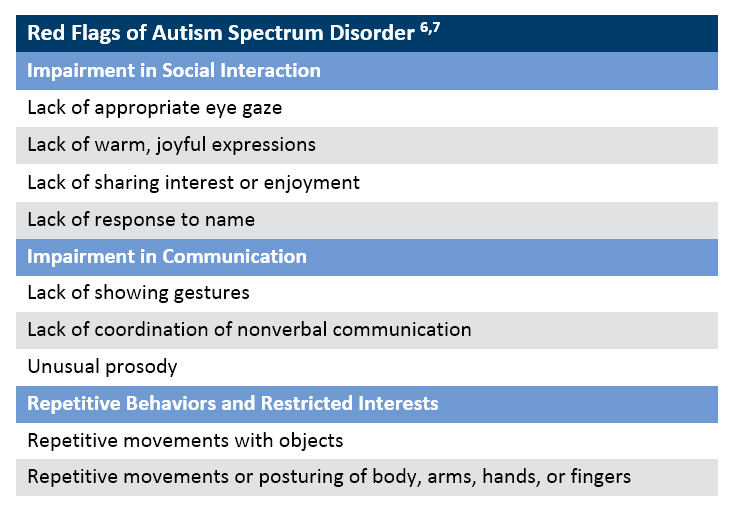
A major challenge to diagnosing ASD is that it currently cannot be determined from something as definitive as a blood test. The DSM-5 does provide standardized diagnostic criteria for ASD, which defines the disorder as having both deficits in social communication and having the presence of restricted or repetitive type behaviors. Symptoms of ASD must be present in early development; however, the symptoms may not be obvious until later in a child’s development.5 PAs should look for the “red flags” of ASD when managing pediatric patients (Chart 1).
Chart 1. Red Flags of Autism Spectrum Disorder
Why is early diagnosis important?
While there currently is no cure for ASD, early intervention treatment services can greatly improve a child’s development and even mitigate the severity of their symptoms. Early intervention targets birth to age 3, and involves a combination of therapy including physical, occupational and speech therapy. Early intervention can improve not only intellectual development, but communication, and behavioral development as well.8, 9 Children who received early intervention maintained developmental gains and had reduced ASD symptom severity even after a 2-year follow-up period.10
Less than half the children identified with autism (43%) received comprehensive developmental evaluations by age 3. Perhaps most concerning, is that the majority (87%) of cases noted developmental concerns in their medical or educational records before age 3.5 The striking delay between the age a reliable diagnosis can be made and when the actual diagnosis is made means that children with ASD might not get the early help they need.2
ASD in the Pediatric Patient Population
The red flags of ASD are critical markers to look for when working with the pediatric population, if children are to be referred for early intervention in a timely manner.11 In a recent AAPA survey, just 15% of PAs indicated that they had a somewhat high to high understanding of the red flags. About half (49%) were interested in improving their skills to high or very high (AAPA, unpublished data, 2018).
Medical providers such as PAs are often the first point of contact for caretakers of children with ASD and as such, need to be comfortable speaking about how to identify red flags of ASD, and where to refer caretakers if there is any concern. Studies that show that parents of children with ASD frequently recognize and report concerns in development before their child’s first birthday.12,13
In order to make a diagnosis as early as possible, it is key for PAs to communicate with caretakers about how to identify early flags of ASD and encourage them to vocalize any concerns. AAPA’s survey indicated that only half of PAs (56%) were comfortable discussing ASD with caretakers when there was a concern. When concern is raised, PAs need to be able to facilitate next steps and know where to refer caretakers for further evaluation. Results show that only 1 in 4 PAs who see children ages 0 to 17 years reported knowing where to make referrals for early intervention (22.4%), audiologic evaluation (27.3%), and other further evaluation (22.8%) (AAPA, unpublished data, 2018).
ASD in the Adult Patient Population
ASD is a life-long disability that, depending on the severity of symptoms, differs in the intensity of care needed. Along with symptom management, ASD is often co-morbid with disorders that may require long-term care and monitoring. Epilepsy for example, is co-occurring in 20-30% of autistic adults, and even more common if an intellectual disability is present. Other disorders comorbid to those with ASD include gastrointestinal disorders, psychiatric disorders, and metabolic syndrome.12 The care for ASD does not stop with diagnosis or even with intervention, yet only 35.4% of PAs surveyed responded that they were adequately trained in either their PA program or elsewhere to provide care to patients with ASD (AAPA, unpublished data, 2018). Healthcare providers need the skills and knowledge of comorbidities to be able to care for this increasing prevalent, life-long disorder.
Authors are Noël Smith, MA, AAPA’s senior director of research, and Elaine Slaven, AAPA’s research associate. Contact them at [email protected].
References
- Sandin S, Lichtenstein P, Kuja-Halkola R, Hultman C, Larsson H, Reichenberg A. The Heritability of Autism Spectrum Disorder. JAMA. 2017;318(12):1182. doi:10.1001/jama.2017.12141.
- What is Autism? Autism Science Foundation. https://autismsciencefoundation.org/what-is-autism/. Accessed March 23, 2018.
- Autism Spectrum Disorder (ASD). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/autism/facts.html. Published March 28, 2016. Accessed March 23, 2018.
- Christensen DL, Baio J, Braun KV, et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveill Summ 2016;65(No. SS-3)(No. SS-3):1–23.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- Red Flags. http://www.firstsigns.org/concerns/flags.htm. Accessed March 23, 2018.
- Wetherby AM, Woods J, Allen L, Cleary J, Dickinson H, Lord C. Early Indicators of Autism Spectrum Disorders in the Second Year of Life. J Autism Dev Disord. 2004;34(5):473-493. doi:10.1007/s10803-004-2544-y.
- Dawson, G, Rogers, S, Munson, et al. (2010). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics, 125(1), e17-e23.
- Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol. 1987;55(1):3-9. doi:10.1037//0022-006x.55.1.3.
- Estes A, Munson J, Rogers SJ, Greenson J, Winter J, Dawson G. Long-Term Outcomes of Early Intervention in 6-Year-Old Children With Autism Spectrum Disorder. J Am Acad Child Adolesc Psychiatry. 2015;54(7):580-587. doi:10.1016/j.jaac.2015.04.005.
- Kozlowski AM, Matson JL, Horovitz M, Worley JA, Neal D. Parents’ first concerns of their child’s development in toddlers with autism spectrum disorders. Dev Neurorehabil. 2011;14(2):72-78. doi:10.3109/17518423.2010.539193.
- Bolton PF, Golding J, Emond A, Steer CD. Autism Spectrum Disorder and Autistic Traits in the Avon Longitudinal Study of Parents and Children: Precursors and Early Signs. J Am Acad Child Adolesc Psychiatry . 2012;51(3). doi:10.1016/j.jaac.2011.12.009.
- Nicolaidis C, Kripke CC, Raymaker D. Primary Care for Adults on the Autism Spectrum. Med Clin North Am. 2014;98(5):1169-1191. doi:10.1016/j.mcna.2014.06.011.
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



