PAs Providing Care at the Bottom of the World
An Emergency Medicine Adventure in Antarctica
By Hillel Kuttler
PA Cliff Leonard is Texan as Texan can get. He can spin a yarn, turn a memorable phrase and was born in Corpus Christi. Now he lives in Galveston, a long, narrow barrier island about 50 miles south of Houston.
Immortalized in a Glen Campbell song and the New York Times bestseller “Isaac’s Storm,” Galveston is best known for the 19th-century elegance of its historic districts, tourism and warm sea breezes. At the height of winter, the island’s average low temperature is 49 degrees F.
So what possessed Leonard, who has lived most of his life in warm-weather climates, to brave the frostbite-inducing, subzero temperatures of an island off the coast of Antarctica?
In a word — adventure.
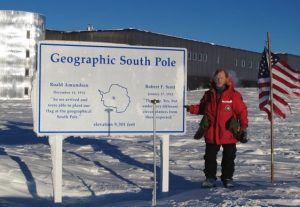
Leonard is among the PAs who’ve traveled to the bottom of the world over the past decade to provide care to the researchers at the South Pole through the Center for Polar Medical Operations (CPMO). Part of the National Science Foundation’s U.S. Antarctic Program (USAP), the center is operated by the University of Texas Medical Branch (UTMB) at Galveston. The center oversees the staffing and healthcare services for the U.S. research stations in Antarctica.
“I found out about this job, and I couldn’t resist,” said Leonard, who heard about an opening at the South Pole and ended up working there from February to October 2013.

Retired after 27 years at UTMB, he found it the perfect time to travel to the South Pole. A 1982 graduate of the Augusta University PA program, he was 60 when he pulled up stakes to travel to McMurdo Station, one of three U.S. research stations in Antarctica.
“I just lived it,” Leonard, now 63, said recently. “It was wonderful. I feel very blessed to have had that experience. Flying between mountains, landing on glaciers, being where very few people have been — the experience of being in the middle of nowhere.”
Adaptability and collaboration is a must
PA Melanie Troftgruben seems ideally suited to adapting seamlessly to living in frozen, wind-swept Antarctica. A PA in emergency medicine, she was raised in North Dakota, has worked in Alaska and now resides in Bozeman, Mont.
The frigid winters in those places haven’t fazed her, which might explain why she’s served three — count them, three — eight-month stints over the past decade to provide medical care for those working at the McMurdo Station, the largest of three American scientific facilities in Antarctica, all run by the National Science Foundation.
Because harsh temperatures are second nature, Troftgruben had to stop and consider a question about what medical conditions she’s treated that are unique to that continent. “It’s hard, because I come from a cold climate, so I didn’t find things you wouldn’t find in a cold climate,” she said.

And Antarctica is cold.
“When I was at the South Pole, the temperature got down to minus 106.7 degrees F,” Leonard said. “I once took pictures when it was minus 104.5 degrees F with a wind chill of minus 145 degrees F.”
The climate and remote location to the research stations make the presence of Troftgruben and other medical staff posted there critical to the health and safety of the scientists and other staff: approximately 1,100 people in the summer and a quarter of that number most winters.
The researchers come to Antarctica to study such matters as the terrain — the vast ice sheets are more than a mile deep — the subterranean lakes, pollution and wildlife (prominently penguins, whales and seals) native to the region. Officials from the National Oceanic and Atmospheric Administration come to learn about Antarctica’s extreme weather.
The remoteness and the conditions make teamwork vital.
Because of the vast distances between Antarctica and the nearest populated areas in New Zealand and Chile, along with the challenges of landing planes on the continent during winter, most medical emergencies must be addressed on site, including at the stations’ urgent-care units. The well-stocked clinics include X-ray machines, ultrasound machines, respirators, ventilators and EKG machines — but not CT or MRI scanners. The PAs, physicians and NPs working at the sites must do it all: draw patients’ blood, hook up IVs, help with physical therapy.
Everyone — medical and nonmedical people alike — trains in emergency response. One drill teaches how to assist someone suffering from exposure who is far from the nearest building: strapping him or her in a Nansen sled behind a snowmobile to be brought in for treatment.
The collaboration applies beyond the clinics’ walls, too. Everyone pitches in to clean, mop, even set up runway lights on the airstrips to guide arriving planes.
“I enjoyed the environment — doing your own X-rays and processing and reading them. You do your own labs and ultrasounds. You need to be a jack of all trades, with a lot of physician backup and telemedicine,” said Troftgruben. “You learn more about yourself, which is a good thing.”
Emergency medicine king of the mountain
What types of PAs are sought? James McKeith, MD, the chief medical officer for the CPMO, wants those with backgrounds in family medicine and emergency medicine who can think independently. He oversees the center at UTMB.

The CPMO seeks health professionals with a background in emergency medicine or experience in remote medical care delivery to treat the USAP participants who travel to Antarctica each year. McKeith is always looking for talented, adventurous and resourceful providers.
Everyone recruited to work in Antarctica is screened to weed out those with serious medical conditions that could flare up in the middle of nowhere.
“We try to select a healthy population,” McKeith said.
A diabetic, for example, could be included in the staff if the person’s condition is well controlled. “We generally try to get healthy people down there, and we work on keeping people healthy,” McKeith said.
That is done with the basics: promoting handwashing and other good hygiene, providing mandatory flu shots (and tetanus, measles, mumps and rubella shots for those who are not immune) and monitoring food-storage conditions.
When Leonard worked at the South Pole, he taught first-aid courses that included everything from treating someone with frostbite and bandaging a wound to more serious medical emergencies, such as how to respond to a heart attack. All of which were well within his bailiwick as a clinician trained to be a medical generalist.
Over the course of his career as a PA, he specialized in orthopaedics, nephrology, ophthalmology and psychiatry. He’s worked in an HIV/AIDS clinic, an ICU, and the prison hospital at UTMB.
“I can’t tell you how much I enjoyed the teaching part,” said Leonard, who’d never before led such courses.
Harsh conditions, hardy clinicians
Working in Antarctica isn’t for everyone.
The general ethos is, “You’re on your own,” PA Scott Deaton said via satellite telephone in September, shortly before he concluded a nine-month stint at the South Pole. “It’s much more hands-on.”
Deaton was speaking just after his clinic opened for the day at 7:30 a.m., a whopping 16 hours ahead of Eastern Standard Time. His workload isn’t typical of what he’d dealt with as a PA in emergency medicine and in oncology back in Portland, Ore.

People catching colds — that’s rare in Antarctica, occurring, he explained, only when new people enter the environment (like staff flown in to commence their rotations) and introduce their viruses. Frostbite doesn’t strike much, either, Deaton and others interviewed said, because everyone is cognizant of the danger and dresses appropriately. Extreme cold-weather gear — boots with 3-inch foam soles, fleece layers, snowpants and bib, goose-feather coats, face and neck masks — is issued.
Clinic visits tend to relate to primary care. Twisted ankles and other injuries resulting from spills on the ice are common. Deaton mostly deals with patients experiencing problems sleeping due to prolonged sun deprivation in winter and sun exposure in summer.
When major issues arise, the healthcare professionals avail themselves of telemedicine capabilities — email, telephone and video chat — with UTMB physicians.
Last June, two people were evacuated together by plane: one with a cardiac condition, the other with a gastrointestinal problem. In the first case, a cardiac ultrasound was performed at the South Pole, which a cardiologist at UTMB observed in real time. The satellite transmission cut out, so the procedure was recorded and transmitted for review. The decision was then made to fly the patients to Chile for care.
“It was a several-week-long process. There were planes that could land here. Unfortunately, they were in Canada,” Deaton recalled. “We had to plow a runway. We managed the patients until the plane could arrive. We spoke to the medical side in the States. The doctor and I were doing 24-hour days: 12 and 12. … It was a relief when they arrived to the coast and from there to Chile. We knew that they were safe.”
Serving at the South Pole meant that Deaton has now traveled to all seven continents.
At sunset — meaning, when winter arrives and the sun departs for many months — “the stars come out, and you can see the [aurora australis]. It’s fascinating to see the changes, the varying light levels,” he said. “It gets very dark, but with all the stars and the aurora, and with all the ice and a full moon, you can go and cast a shadow on the ice.”
For Leonard, the uniqueness of his surroundings prompted him to earn membership in the 300 Club, sitting in a sauna at 200 degrees F, then venturing outdoors to the South Pole marker at minus 100 degrees F. Naked.
“My brain was going, ‘What the hell are you doing?’ ” he said. “That was one of the most exhilarating, insane experiences I’ve ever had. I have a certificate to prove it.”
Troftgruben, too, possesses a certificate attesting to her successful stay in Antarctica. It’s a marriage certificate. On her first assignment there, she met the man who became her husband: Rex Cotten, an information technology specialist.
Coincidentally, Troftgruben’s husband was back at McMurdo Station when PA Professional reached her for this article.
Working in the South Pole gets into your blood. Troftgruben can’t wait to go back in a few months. “I will be returning for the winter contract in February 2017,” she said.
Hillel Kuttler is a freelance writer and editor who has written about PAs and healthcare for many years. He can be reached by email.
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.