AAPA Response to AMA’s #StopScopeCreep Campaign
November 2, 2020
Susan R. Bailey, MD
President
James L. Madara, MD
Chief Executive Officer & Executive Vice President
American Medical Association
AMA Plaza
330 N. Wabash Ave., Suite 39300
Chicago, IL 60611-5885
Dear Drs. Bailey and Madara,
 On behalf of the more than 140,000 PAs across this country who work alongside physicians in every medical setting and specialty, we ask that the American Medical Association (AMA) cease advancing the false and offensive narrative in your #StopScopeCreep campaign, which suggests PA care is not safe and jeopardizes patient safety.
On behalf of the more than 140,000 PAs across this country who work alongside physicians in every medical setting and specialty, we ask that the American Medical Association (AMA) cease advancing the false and offensive narrative in your #StopScopeCreep campaign, which suggests PA care is not safe and jeopardizes patient safety.
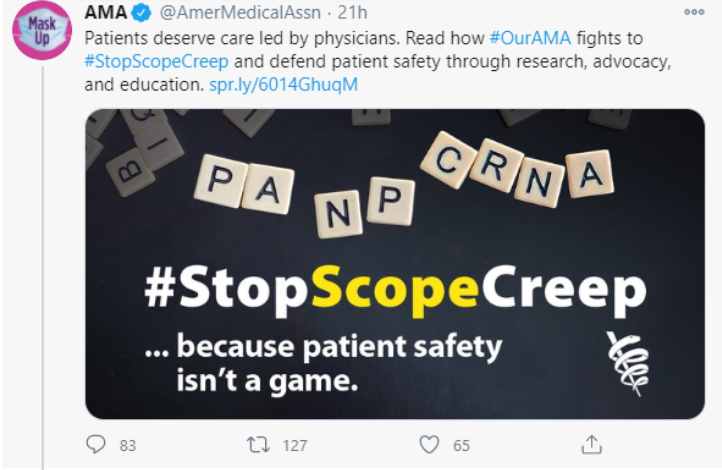
While this misleading narrative from AMA is not new, we are writing today with a renewed sense of urgency. Over the weekend, AMA posted particularly ill-timed social media messages that have since been deleted. These messages denigrated the PA profession and misled the public.
The COVID-19 pandemic has made this year especially challenging for all medical providers. Three out of five PAs have tested, treated, and diagnosed COVID-19 patients. Like physicians, PAs have experienced furloughs, layoffs, reduced hours—and have contracted and died from the virus. So, AMA’s whimsical graphic with the PA profession represented on Scrabble tiles with the message “because patient safety isn’t a game” was unconscionable.
Most egregious is AMA’s tone-deaf attempt to instill more fear and uncertainty in the public at a time of already heightened anxiety. As we have seen across the country, patients continue to delay life-saving care due to COVID-19. Using scare tactics to disincentivize patients from accessing healthcare during a pandemic is disconcerting and reckless to public health.
Our professional organizations should work together to find solutions to current healthcare challenges, for example, increasing acceptance and delivery of vaccines. We should focus on combatting misinformation, such as the recent suggestions that physicians and other clinicians are falsely attributing deaths to COVID-19. We should build public confidence in our nation’s healthcare workforce. Instead, your organization is attempting to divide rather than unite by attacking other healthcare providers.
Your assertion that a patient’s safety is at risk if they see a PA is simply false and AMA’s continued efforts to suggest otherwise are deceitful. Study after study confirms that PAs provide high-quality care.1-2 In fact, additional studies find that PAs have similar health outcomes as physicians.1,3-5
We would also like to address the AMA’s antiquated concept of “physician-led patient care and training.” This is not only contrary to what evidence shows is best for patients but is also out of touch with how medicine is practiced today. The most up-to-date practice laws allow healthcare teams to decide at the practice level how they will collaborate to best meet the needs of patients. Evidence demonstrates the most successful clinical teams are those that utilize the skills and abilities of each team member most fully, and a team approach supports efficient patient-centered healthcare.6-8 The keyword is “team.”
PAs, like physicians, seek to reduce unnecessary and outdated administrative burdens that limit patient care. Removing the legal tether, such as a practice agreement between a PA and another specific healthcare provider, allows healthcare teams to be more flexible in meeting patient care needs. This was most recently evidenced during the pandemic when the governors of eight states removed supervision requirements for PAs and another 13 did so through previous legislation specific to PA practice during a public health emergency. PAs did what they were trained to do: go where they are needed most.
Whether during a pandemic or not, PAs will continue to collaborate with, consult with, and refer patients to other healthcare providers whenever the patient’s condition falls outside of their education, training, and experience.
It is also worth noting that removing this legal tether has many benefits to physicians, something which AMA should explain to its members. These benefits include removing physician liability for the care that PAs provide when physicians are not involved and reducing physician and employer risk of disciplinary action for administrative reasons.
PAs have great respect for the breadth and depth of physician training and are proud to practice medicine alongside physicians every day. We ask for mutual respect and for AMA to not hide behind inflammatory social media messages.
We would like to meet with AMA leaders to clear up any misperceptions and to begin working together toward improving and expanding access to high-quality care for patients. We look forward to the opportunity to further this conversation.
Beth R. Smolko, DMSc, MMS, PA-C
President and Chair of the Board
American Academy of PAs
Lisa M. Gables, CPA
CEO
American Academy of PAs
References
- Kurtzman ET, Barnow BS. A Comparison of Nurse Practitioners, Physician Assistants, and Primary Care Physicians’ Patterns of Practice and Quality of Care in Health Centers. Med Care. 2017;55(6):615-622. doi:10.1097/MLR.0000000000000689.
- U.S. Department of Health and Human Services, Health Resources and Services Administration. National Practitioner Data Bank. Rockville, MD: U.S. Department of Health. https://www.npdb.hrsa.gov/index.jsp. Accessed November 2, 2020.
- Jackson GL, Smith VA, Edelman D, et al. Intermediate Diabetes Outcomes in Patients Managed by Physicians, Nurse Practitioners, or Physician Assistants: A Cohort Study. Ann Intern Med. 2018;169(12):825-835. doi:10.7326/M17-1987.
- Rymer JA, Chen AY, Thomas L, et al. Advanced Practice Provider Versus Physician-Only Outpatient Follow-Up After Acute Myocardial Infarction. J Am Heart Assoc. 2018;7(17):e008481. doi:10.1161/JAHA.117.008481.
- Yang Y, Long Q, Jackson SL, et al. Nurse Practitioners, Physician Assistants, and Physicians Are Comparable in Managing the First Five Years of Diabetes. Am J Med. 2018;131(3):276-283.e2. doi:10.1016/j.amjmed.2017.08.026.
- Mitchell PM, Wynia R, Golden B, et al. Institute of Medicine. Core principles and values of effective team-based health care. https://nam.edu/perspectives-2012-core-principles-values-of-effective-team-based-health-care. Published October 2, 2012. Accessed November 2, 2020.
- Doherty RB, Crowley RA; Health and Public Policy Committee of the American College of Physicians. Principles supporting dynamic clinical care teams: an American College of Physicians position paper. Ann Intern Med. 2013;159(9):620-626. doi:10.7326/0003-4819-159-9-201311050-00710.
- Jabbarpour Y, DeMarchis E, Bazemore A, Grundy P. The impact of primary care practice transformation on cost, quality, and utilization: A systematic review of research published in 2016. Washington, DC: Patient Centered Primary Care Collaborative. https://www.pcpcc.org/sites/default/files/resources/pcmh_evidence_report_08-1-17%20FINAL.pdf. Published July 2017. Accessed November 2, 2020.
Click here for the PDF version of this letter.
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.